Etiology
- Mitral valve prolapse, due to
- Degenerative (myxomatous) disease
- Connective tissue disorders (Marfan’s, Ethlers-Danlos)
- Congenital abnormalities
- LV dilation
- Damage to valve cusps/chordae – rheumatic heart disease, endocarditis
- Papillary muscle dysfunction
- MI
Pathophysiology
Chronic MVR
- causes gradual dilation of LA, with little increase in left atrial pressure (LAP)
- Therefore has few symptoms at first
- LV dilates slowly due to the chronic volume overload of the LV due to regurgitation
- LVDP and LAP gradually increase
Acute MVR
- LA compliance is normal so doesn’t dilate
- So LAP rises
- Leads to ↑pulmonary venous pressure and pulmonary oedema
- SV decreases due to regurgitation
- So LV hypertrophies to increase SV and therefore CO
MV prolapse – MCC of mild MVR
- In mild MV prolapse the valve remains competent but bulges back into the LA during systole
- Causing a mid-systolic click but no murmur
 Severe MV prolapse causes regurgitation
Severe MV prolapse causes regurgitation
- Click is followed by a late-systolic murmur
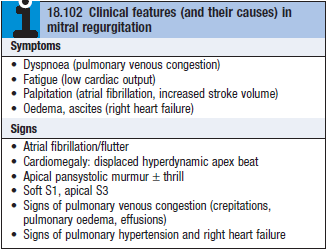
Clinical features
- Chronic MVR – similar symptoms to MVS
- Acute MVR – causes acute pulmonary oedema
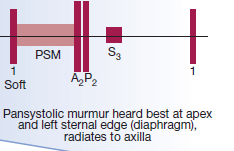
- Apical systolic murmur – due to regurgitant jet
- Loud S3
- Displaced active apex beat – due to LV volume overload and LV dilation
Investigations
ECG
- LA hypertrophy
 LVH
LVH
CXR
- Enlarged LA + LV
- Pulmonary venous congestion
Echo
- Dilated LA, LV
- Structural abnormalities of MV – e.g. prolapse
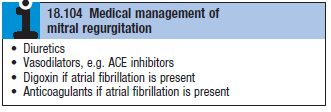
Management
- If MVR is moderate then it can be treated medically (see box)
- MV repair – to treat prolapse
- CABG – if MVR is accompanied by ventricular dilation and dysfunction
