- Shock – clinical syndrome that develops when there is critical impairment of tissue perfusion due to some form of acute circulatory failure
- Cardiogenic shock – failure of pumping action of the heart, resulting in ↓CO, and ↓end-organ perfusion
- Presence of the following (despite adequate LV filling pressure)
 Sustained hypotension – SBP<90mmHg for >30 mins
Sustained hypotension – SBP<90mmHg for >30 mins- Tissue hypoperfusion – cold peripheries, oliguria
- MCC – LHF > pulmonary congestion > hypoperfusion
- Presence of the following (despite adequate LV filling pressure)
Etiology
- Acute MI – MC
- Arrhythmias
- Cardiac rupture
- Acute PE
- Cardiac tamponade
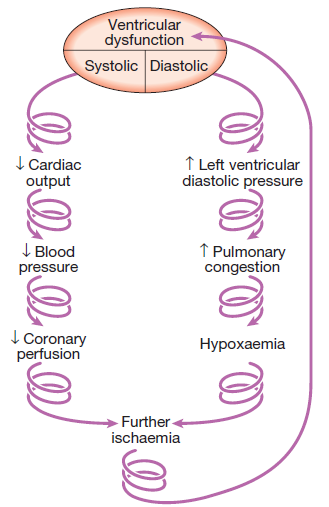
Pathophysiology – see diagram
- ↓ coronary perfusion pressure and CO and ↑ myocardial oxygen demand
- Create a vicious cycle that leads to cardiogenic shock
Clinical features
- Chest pain, N + V, dyspnoea, sweating, palpitations
- Pale, cold skin
- Poor peripheral pulses
- Hypotenison
- Tachy/bradycardia, murmurs
- Pulmonary crackles
- Oliguria
- Altered mental state
Management
- ABC
- Airway + breathing – intubation/mechanical ventilation if needed; oxygen
- Circulation – gain venous access to take blood for investigation and administration of IV fluids
- Monitor vital signs
- Pulse, BP, respiratory rate, O2 sats
- Insert urinary catheter
- Investigations
- U+E, creatinine
- LFTs
- Cardiac enzymes, ECG, CXR, Echo
- FBCs
- ABGs
- BNP
- Inotropic drugs – Vasopressors (adrenaline, dobutamine)
- Revascularisation
If CO is inadequate and contractility is poor
- Reduce afterload
- Hydralazine [25mg t.i.d]
- Intra-aortic balloon bump counterpulsation (IABP) – reduces afterload, increases CO and coronary perfusion
- Increase preload
- Improve contractility – inotropes (see above)
- Control rate and rhythm
- Correct hypokalaemia and hypomagnesaemia
- IV amiodarone – to control ventricular rate and restore sinus rhythm
