1. ANATOMY
2. GASTRIC ULCER
Epidemiology/Etiology
- Imbalance between protective and damaging factors of gastric mucosa
- Atrophic gastritis, bile reflux, gastric stasis, abnormalities in acid and pepsin secretion
- Smoking, alcohol, NSAIDs, steroids
- H. Pylori
- Low socioeconomic group
Pathogenesis
Factors involved in gastric ulcer formation
- Duodenogastric reflux – contains bile salts and lysolecithin
- Breaks the mucosal barrier making it more vulnerable for injury
- Ischemia of gastric mucosa
Pathology
- The ulcer’s floor is formed by the muscular layer
- Posteriorly it can penetrate into the pancreas
- Can cause torrential bleeding by eroding left gastric or splenic arteries
- Anteriorly it can perforate into the liver – causing hour glass contracture or tea-pot deformity
- Microscopic – ulcer crater with chronic inflammatory cells, granulation tissue and epithelial proliferation
- Grossly, margin of benign ulcer is clear, deep, near lesser curvature
- Gastric ulcer >3cm has a higher chance of malignant transformation
- 95% of benign gastric ulcers occur toward the lesser curvature as it takes more burden of passage of food, therefore more wear and tear
- Acute ulcer – confined to mucosa and submucosa. Due to NSAIDs
- Chronic ulcer – penetrates muscularis layer of stomach
Classification of Types of Gastric Ulcer – Daintree Johnson Classification
- Type I – in the antrum, near the lesser curvature (normal acid level)
- Type II – combined gastric and duodenal ulcer (high acid level)
- Type III – prepyloric ulcer (high acid level)
- Type IV – ulcer in the cardia or proximal stomach (normal acid level)
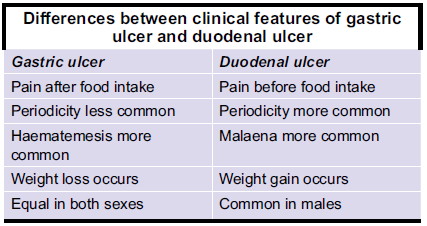
Clinical Features
- Pain in epigastric region after food
- Relieved by vomiting
- Periodicity – symptom free interval for 2-6 months
- Weight loss
- Aversion to spicy, fried foods
Investigations
- Barium meal XR – to see niche and notch
- Gastroscopy – location, type of ulcer, biopsy
- US abdomen – rule out other disease
Differential diagnosis
- Hiatus hernia, cholecystitis, chronic pancreatitis, dyspepsia, carcinoma stomach
Treatment
- H2 blockers – promote ulcer healing by reducing acid secretion
- Cimetidine, ranitidine, famotidine (most potent)
- Proton pump inhibitors – inhibits parietal cell H+/K+ATPase enzyme responsible for acid secretion
- Omeprazole, lansoprazole, pantoprazole
- Surgery – partial gastrectomy and Billroth I gastroduodenal anastomosis
- Type IV proximal ulcer is difficult to manage – treated by subtotal gastrectomy
- Pauchet’s procedure – sleeve like extension cut along the lesser curve to remove the ulcer
Complications
- Hour glass contracture – the stomach is divided into two compartments
- Clinical features – loss of periodicity, persistent pain, vomiting, loss of appetite and weight
- Diagnosis – barium meal, shows filling only in the proximal stomach
- Treatment – partial gastrectomy and Billroth I anastomosis is done
- Tea-pot deformity (hand-bag stomach) – due to cicatrisation and shortening of lesser curve
- Perforation
- Bleeding – erosion into left gastric and splenic arteries. Most common in type II and III ulcers
- Penetration – posteriorly into pancreas and anteriorly into liver
- Malignant transformation – adenocarcinoma of stomach is the most common
3. DUODENAL ULCER
Epidemiology/Etiology
- Most common in blood group O +ve
- Stress, anxiety
- H.pylori infection
- NSAIDs, steroids
- Endocrine causes – Zollinger-Ellison syndrome , MEN syndrome , hyperparathyroidism
,
Pathogenesis
- Duodenal ulcers occur in first part of duodenum – involve the muscular layer
- Eventually shows cicatrisation causing pyloric stenosis
- Serosa overlying the site of ulcer shows petechial haemorrhages with speckled red dots – cayenne pepper
- Microscopic – chronic inflammation with granulation tissue, gastric metaplasia of duodenal mucosa
- Kissing ulcers – 2 opposing ulcers, one over the anterior surface and one over the posterior surface of the duodenum
- Anterior ulcer perforates commonly
- Posterior ulcer bleeds or penetrates commonly
Clinical features
- Pain relieved by food – increased appetite so patients are more likely to gain weight
- Night pains are common
- Heart burn and vomiting
- Periodicity is more common than in gastric ulcer
- Melaena, haematemesis
Investigations
- Barium XR – deformed or absent duodenal cap
- Gastroscopy – type and location of ulcer; biopsy to look for H.pylori
- Serum gastrin level
Treatment
- General measures – avoid alcohol, NSAIDs, smoking, spicy food
Drugs
- H2 Blockers
- Proton pump inhibitors
- Antacids – neutralise HCl to form water and salt
- Aluminium hydroxide
- Sucralfate – aluminium salt which provides protective coat to ulcer crater and promotes healing
- Anti H.pylori regimen – triple therapy
- Omeprazole, clarithromycin, amoxicillin
Surgery
- Highly selective vagotomy (HSV)
- Only fibres supplying the parietal cells are ligated, reduces acid secretion so ulcer heals
- Truncal vagotomy with gastrojejunostomy
Complications
- Pyloric stenosis – due to scarring of first part of duodenum
- Bleeding, perforation
- Penetration into pancreas
- Residual abscess