1. PYOGENIC LIVER ABSCESS
Etiology
- Abscesses arise in the liver as a result of bacterial infection
- Potential routes of hepatic exposure to bacteria
- Biliary tree, portal vein, hepatic artery, direct spread, trauma
- Most common organisms
- E.coli, K.pneumoniae, S.aureus, Enterococci, Bacteroides
Pathogenesis
- Infection from the biliary tree – most common cause
- Biliary obstruction leads to bile stasis – this creates nidus for bacteria colonisation
- Infection can then ascend to the liver – ascending suppurative cholangitis
- Portal vein sepsis
- Portal vein drains the GIT – so any infection of GIT can cause ascending portal vein infection
- E.g. Diverticulitis, appendicitis, pancreatitis, inflammatory bowel disease (IBD), pelvic inflammatory disease
- Systemic infections through hepatic artery
- Endocarditis, pneumonia, osteomyelitis, bacteraemia
- Direct extension of a nearby infection
- Suppurative cholecystitis, subphrenic abscess, perforation
- Penetrating/blunt trauma – form haematoma and necrosis of liver
Pathology
- 75% cases involve the right lobe due to preferential laminar blood flow and larger blood supply
- Abscesses can coalesce to give a honeycomb appearance
Clinical features
- Right upper quadrant pain, fever
- Jaundice – in a third of patients
- Hepatomegaly
- General malaise, chills
- Pleural effusion
Investigations
- Blood – ↑ALP, leukocytosis, ↑ESR
- CXR – elevated right hemidiaphragm, right sided pleural effusion
- US – shows round/oval hypoechoic areas
- CT
Treatment
- Broad spectrum antibiotics – start empirically until culture is available
- Should cover gram negative and anaerobic bacteria – 3rd generation cephalosporins, metronidazole, aminoglyosides
- Percutaneous drainage of abscess under US guidance
2. AMOEBIC LIVER ABSCESS
Epidemiology/Etiology
- Entamoeba Histolytica – exists as cysts in a vegetative form, capable of surviving outside the human body
- Prevalent in tropical climates, especially in areas with poor sanitation
- More common in alcoholic/cirrhotic patients
- Transmission is via the faecal-oral route
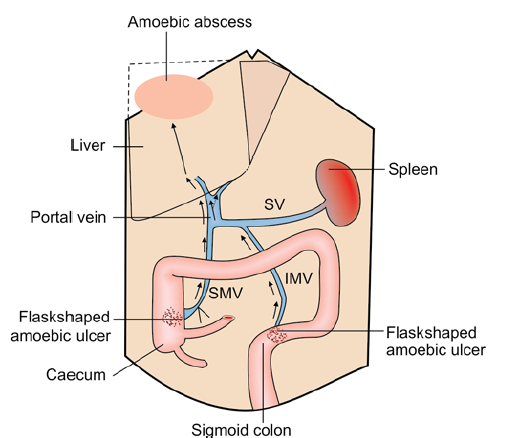
Pathogenesis
- Cyst is swallowed via food/water that is contaminated with faeces – the cyst is resistant to gastric acid
- It then enters small intestine undamaged and reaches distal ileum/caecum where the trophozoite is released and multiplies
- It infects the liver through the inferior mesenteric or portal vein (see pic)
- Trophozoites destroy hepatocytes by releasing histiolysin – cause amoebic hepatitis and multiple microabscesses
- It can resolve spontaneously or lead to a localised amoebic liver abscess
- Abscess is more common in right posterior-superior region of the liver
- Liquefaction necrosis occurs which forms a thick chocolate brown pus (anchovy sauce)
- Consists of dead hepatocytes, RBCs, and necrotic material
 There is risk of rupture and spread
There is risk of rupture and spread
Course of abscess and consequences
- Rupture into lungs – leads to chocolate coloured sputum
- Rupture into peritoneum – peritonitis (emergency)
- Rupture into pleural cavity – empyema
- Rupture into bronchus – bronchopleural fistula
- Rupture into skin – amoebiasis cutis
- Rupture into pericardial cavity – cardiac tamponade (high mortality)
- Septicaemia in patients with cirrhosis
Clinical features
- High fever, sweating, weight loss, cough
- Right upper quadrant pain and tenderness
- Leukocytosis
- Right sided pleural effusion
- Amoebic dysentery
Investigations
- US, CT – raised diaphragm, abscess cavity, size, location, presence of effusion
- XR – raised fixed diaphragm, pleural effusion, soft tissue shadow
- LFTs
- Aspiration – microscopy
- PCR
Treatment
- Metronidazole 750mg t.d.s for 5-10 days
- IV/oral antibiotics to control secondary infection – cefotaxime, amoxicillin
- US guided aspiration – in the 9th + 10th intercostal space
