Epidemiology
- Pancreatic endocrine tumours can be single or multiple, benign or malignant
- Associated with MEN I syndrome – pituitary, parathyroid and pancreatic neoplasm
Pathology
- The cells of the endocrine portion of the pancreas are Islet cells
- α – secretes glucagon
- β – secretes insulin
- δ – secretes somatostatin
- γ – secrete pancreatic polypeptide
- Tumours of these cells can lead to increase levels of their secretions
Insulinoma
- Most common functional endocrine neoplasm
- Arise from β cells of the pancreas, cause an increase in insulin
- 15% are malignant, 85% are benign
- Can occur in the head, body, and tail of pancreas
- Presents with Whipple’s triad
- Fasting hypoglycaemia
- Serum glucose level <50mg/dL
- Symptoms relieved by glucose
Clinical features
- Abdominal discomfort
- Hunger – overeating can cause weight gain
- Syncope, palpitations, trembling, confusion, seizures
Investigations
- Low blood glucose level
- Insulin >7μU/ml
- Plasma insulin:glucose ratio >0.3 is diagnostic
- C-peptide >1.2μg/ml
- MRI to localise tumour
Treatment
- Enucleation
- Distal pancreatectomy
- Diazoxide – suppresses insulin sec retion
Gastrinoma 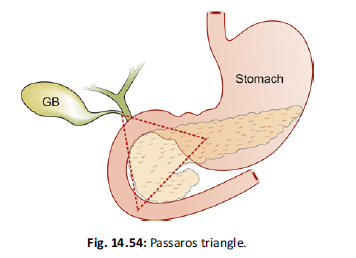
- Arise from G cells of the pancreas which secrete high levels of gastrin
- Most common endocrine pancreatic tumour seen in MEN I syndrome
- Zollinger-Ellison syndrome – caused by gastrinoma in head of pancreas
- Increased gastrin secretion by G cells → hypersecretion of acid by parietal cells → causes peptic ulceration
- Half are multiple and malignant
- Common in Passaros triangle (see pic)
- Three points that form the triangle
- Superiorly – confluence of the cystic and common bile ducts
- Inferiorly – junction of the 2nd and 3rd portions of the duodenum
- Medially – junction of the neck and body of the pancreas
- Three points that form the triangle
Clinical features
- Abdominal pain, diarrhoea, weight loss
- Peptic ulcer disease
- Severe oesophagitis
Investigations
- Serum gastrin levels >1000pg/ml – normal level is 200pg/ml
- Gastroscopy
- MRI/CT
Treatment
- Enucleation
- PPI – omeprazole
- H2 blockers
VIPoma
- VIP (vasoactive intestinal peptide) secreting tumour, most common in the distal pancreas
- Most VIPomas are malignant
- VIP stimulates secretion of water and electrolytes into intestine
Clinical features
- Severe, intermittent watery diarrhoea
- WDHA syndrome – watery diarrhoea, hypokalemia, achlorhydria
- Lethargy, muscle weakness, crampy abdominal pain
Investigations
- Fasting VIP plasma level
- CT scan
- Scintigraphy
Treatment
- Correct dehydration
- Octreotide – somatostatin analogue
- Blocks action of VIP
- Distal pancreatectomy
Glucagonoma
- Arises from alpha cells – causes increase in glucagon
- Commonly malignant – most have metastasised at time of presentation (especially to the liver)
- Most common in the tail of pancreas
Clinical features
- 4D syndrome – dermatitis, diabetes mellitus, deep vein thrombosis (DVT), depression
- Diarrhoea, anemia, weight loss
Investigations
- Serum glucagon >500pg/ml
- MRI/CT
Treatment
- Control diabetes, anemia and nutritional deficiencies
- Prevention of DVT
- Distal pancreatectomy
- Whipple’s procedure – pancreaticoduodenectomy
- Darcarbazine
Somatostatinoma
- Arise from the delta cells – produces somatostatin
- Somatostatin inhibits pancreatic and biliary secretion – leads to biliary stasis
- Somatostatinomas are associated with
- Gallstones and steatorrhoea – inhibition of cholecystokinin
- Diabetes – inhibition of insulin
- Most common site – head of pancreas and peri-ampullary area
- Clinical features – abdominal pain, jaundice, gallstones
- Investigations – serum somatostatin >10ng/ml
- Treatment – tumour excision and cholecystectomy
