1. ANATOMY
- Celiac trunk supplies foregut, hepatobiliary system, spleen
- Superior mesenteric artery (SMA) supplies the small bowel, proximal and mid colon
- Inferior mesenteric artery (IMA) supplies the distal colon and rectum
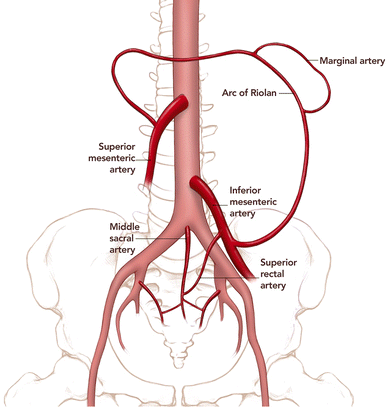
- The GIT has many arterial collateral vessels between all 3 major vessels to protect from gut ischemia
- Collaterals between the celiac trunk and SMA – via the gastroduodenal artery
- Collaterals between the SMA and IMA – via the arc of Riolan and the marginal artery of Drummond
2. GENERAL FEATURES OF ACUTE MESENTERIC ISCHAEMIA
- Causes of mesenteric ischaemia
- Arterial – embolism, thrombus, non-occlusive
- Venous thrombosis
- Regardless of the cause, acute mesenteric ischaemia can lead to intestinal mucosal sloughing within 3 hours of onset and full-thickness intestinal infarction by 6 hours
- General clinical features
- Generalised abdominal pain – out of proportion to clinical exam
- Initially pain is around the umbilicus, later becomes diffuse and constant
- Nausea and vomiting
- Tenderness
- Rebound tenderness (Blumberg sign)
- Generalised abdominal pain – out of proportion to clinical exam
3. ARTERIAL ISCHAEMIA
Mesenteric Embolism
- Embolism most commonly occurs in the SMA
- It is the most dangerous type of mesenteric ischaemia
Etiology – cardiac origin
- Atrial fibrillation
- Mural infarct
- Endocarditis vegetations
Investigations
- Angiogram
Treatment
- If diagnosis is within 6 hours
- Thrombolytics – streptokinase within 6 hours
- Heparin – to stop formation of new thrombus
- Diagnosis after 12 hours
- Embolectomy
- Surgery with intestinal resection
Mesenteric thrombosis
- Most common in the inferior mesenteric artery (IMA)
Etiology
- Atherosclerosis
- Buerger’s disease
Pathogenesis/clinical features
- Thrombus formation leads to decreased blood supply, however there is development of collaterals
- Abdominal angina – pain after eating
- Because there is a threefold increase in blood requirement during digestion, so ischemia occurs faster and causes pain
- Vomiting, diarrhoea, dehydration
- As patient deteriorates – oliguria, abdominal distension, metabolic acidosis
- In severe cases – perforation, peritonitis, ileus
Investigations
- Angiogram
Treatment
- Transcatheter therapy
- Surgical exploration – for necrosis
Non-occlusive mesenteric ischaemia
- Diffuse, intense splanchnic arterial vasospasm
Etiology – systemic hypoperfusion due to several causes
- Shock – cardiogenic, hypovolemic or septic shock
- Post operative – cardiac or abdominal surgery
- Blunt abdominal trauma
- Medication induced mesenteric vasospasm – digoxin, amphetamines, cocaine
Investigations
- Mesenteric angiogram
Treatment
- Antispasmodics – papaverine
- Vasodilators
- Heparin
4. MESENTERIC VENOUS THROMBOSIS
- Thrombosis of the superior mesenteric or portal vein can be due to two main mechanism
Descending/central mechanism
Etiology – due to low flow states in the mesenteric venous circulation
- Portal hypertension
- Liver cirrhosis
- Congestive heart failure
- Autoimmune vasculitis
- Congenital hypercoagulable states – e.g. thrombophilia, protein C and S deficiency
Clinical features
- Diffuse pain
- Patients can have symptoms for days without ischemia
- Due to development of collateral circulation
Investigations
- CT and Doppler US
Treatment
- Heparin
- Thrombolytics
- If patient presents with acute abdomen then surgery is required
Ascending/peripheral mechanism
- Venous thrombosis associated with intra-abdominal infections from organs that drain into the mesenteric veins
- Appendicitis, diverticulitis, pancreatitis
- Clinical features are usually milder
- Therefore patients are more likely to seek treatment at a later stage when they present with acute abdomen
- By this stage there can be extensive necrosis and peritonitis
