1. HAEMORRHOIDS
- Disrupted and dilated anal vascular cushions
Epidemiology
- Prevalence in US – 4%
- Most common in Caucasians
Etiology
- Excessive straining – chronic constipation, diarrhoea
- Increased intra-abdominal pressure – pregnancy, ascites
- Lack of exercise, diet lacking in fibre, obesity
- Congestion from pelvic tumour
Pathophysiology
- Haemorrhoids are cushions of submucosal tissue containing venules, arterioles and smooth muscle fibres
- Located in the anal canal – part of normal anorectal anatomy
- They function as part of the continence mechanism and aid in complete closure of the anal canal at rest
 Haemorrhoids are attached by smooth muscle and elastic tissue – makes them prone to displacement and disruption
Haemorrhoids are attached by smooth muscle and elastic tissue – makes them prone to displacement and disruption- Effects of gravity, anal tone and straining – makes them bulky and loose
- Protrude and form piles
- Vulnerable to trauma and bleed readily from capillaries
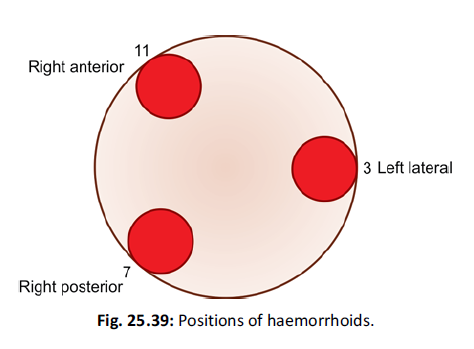
- Positions of haemorrhoidal cushions – see pic
- 11, 3 and 7 o’clock
Types
External
- Located distal to dentate/pectinate line, covered with anoderm
- Anoderm is richly innervated therefore thrombosis of external piles causes pain
Internal
- Proximal to dentate line, covered by insensate anorectal mucosa
- May prolapse/bleed
- Rarely become painful – only when they develop thrombosis/necrosis (strangulation or severe prolapsed)
- Classification
- First degree – don’t prolapse through the anus
- Second degree – prolapse through the anus but reduce spontaneously
- Third degree – prolapse through the anus and require manual reduction
- Fourth degree – prolapse through the anus but cannot be reduced; they are at risk for strangulation
Combined
- Straddle the dentate line
- Characteristics of both
Clinical features
- Features of irritation – pruritis, mucus discharge, discomfort
- Features of damage to mucosal lining – recurrent post-defecatory bleeding (bright red blood)
- Features of prolapse – intermittent lump appearing at anal margin, usually after defecation
Investigations
- Physical exam – usually diagnostic
- Colonoscopy, flexible sigmoidoscopy
- FBC – may indicate anaemia
Complications – Thrombosis, gangrene, fibrosis, strangulation
Treatment
1st and 2nd degree
- Improves with increased fibre and fluid in diet
2nd and 3rd degree
- Non-operative
- Ligation – band strangulates underlying tissue
- Sclerosants – 2ml of 5% phenol injected into piles above dentate line
- Infrared coagulation – coagulates vessels
- Cryotherapy – has high complication rates
- Surgery
- Excisional haemorrhoidoplexy – excision of piles and ligation
- Stapled haemorrhoidoplexy – for prolapsing piles
- Complications – constipation, infection, stricture, bleeding
2. ANAL FISSURES
- Tear in the anoderm distal to the dentate line
Epidemiology
- Males and females are equally affected
- Peak incidence 15-40 yrs
- Can occur in kids due to poor toileting
Etiology
- Initiating factor thought to be from trauma from the passage of hard stools, low fibre diets or previous anal surgery
Pathophysiology
- Tear in anoderm leads to spasm of internal anal sphincter – causes pain, tearing and decreased blood supply to anoderm
- This cycle of pain, spasm and ischemia contributes to the development of a poorly healing wound that becomes a chronic fissure
- Most anal fissures occur in the posterior midline
Clinical features
- Tearing pain with defecation
- Hematochezia – passage of fresh blood in stool
- Intense and painful spasm – lasts for several hrs post defecation
- Lateral location of fissure may indicate underlying disease – Crohn’s disease, HIV, syphilis, TB
Investigations
- Digital and anoscopic exam can result in severe pain – not needed if fissure can be visualised
- If necessary then exam should be done under anaesthesia
Treatment
- Focuses on breaking cycle of pain, spasm, ischemia
Medical
- Stool softeners, warm sitz bath
- 2% lidocane jelly – symptomatic relief
- Nitroglycerine ointment – improve local blood flow
- Calcium channel blocker – diltiazem, nifedipine
- Decreases spasm
Surgical
- For chronic fissures that have failed medical therapy
- Lateral internal sphincterotomy – to decrease spasm of sphincter by dividing a portion of the muscle
