Sustained ventricular tachycardia (VT) (>30 seconds)
 Can result in dizziness, syncope, hypotension, cardiac arrest
Can result in dizziness, syncope, hypotension, cardiac arrest- 120-220 bpm
Etiology
- Occurs in the setting of acute MI, coronary artery disease, cardiomyopathy
- Happens when there is extensive left ventricular (LV) dysfunction
Pathogenesis
- Caused by abnormal automaticity/triggered activity (in ischemic tissue) or re-entry (in scarred ventricular tissue), extra systoles
- VT can cause haemodynamic compromise and can degenerate into ventricular fibrillation
Clinical features
- Palpitations, dizziness, dyspnoea, syncope
ECG
- Rapid ventricular rhythm with broad, abnormal QRS complexes
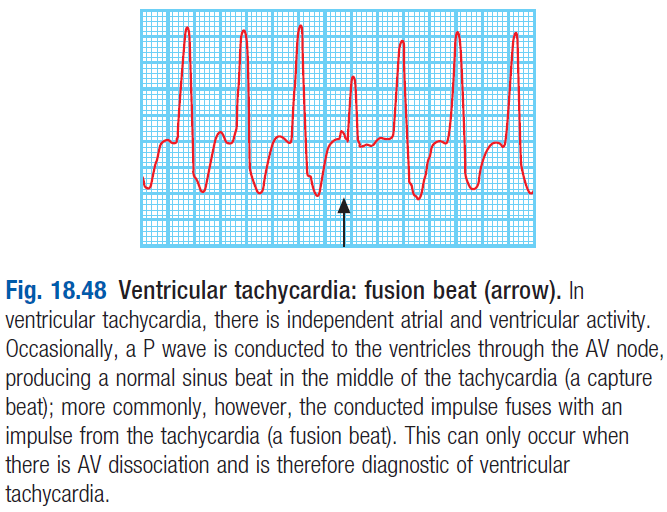
- Features of AV dissociation – results in a fusion beat (see pic)
 relationship between P waves and QRS is lost as ventricles contract independently of atria
relationship between P waves and QRS is lost as ventricles contract independently of atria
Management
- DC cardioversion – to restore sinus rhythm
- IV amiodarone [200mg t.i.d]
- Correct hypokalaemia, hypomagnesaemia, acidosis
- BB – to reduce ventricular automaticity
- ICD – for patients at high risk of arrhythmic death
Ventricular fibrillation (VF)
- Very rapid and irregular ventricular activation with no mechanical effect
- VF is usually provoked by a ventricular ectopic beat (see below)
- Patient is pulseless and becomes rapidly unconscious; respiration ceases
- ECG – shapeless, rapid oscillations with no organised complexes
- Tx – ALS, electric defibrillation. ICD to manage later risk of sudden death
Brugada syndrome
- Inherited condition – idiopathic VF in pts who have no evidence of structural heart disease
- Associated with loss of sodium channel function due to a mutation in the SCN5A gene
- Can present with sudden death during sleep
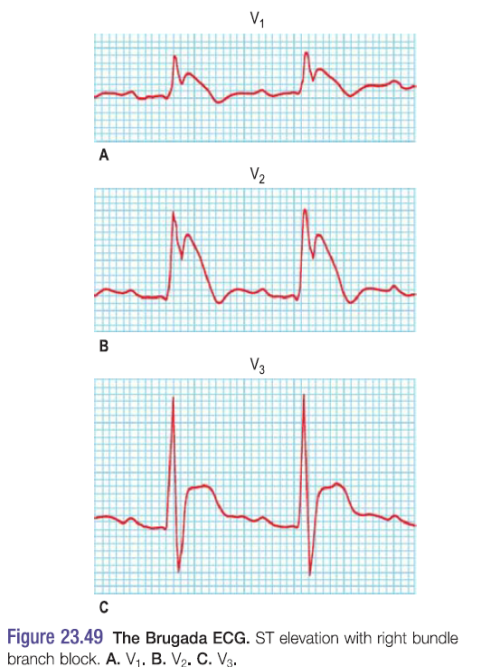
- Dx is by seeing ECG changes
- Ajmaline/flecainide (Class I AA) are administrated to induce arrhythmia in a pt suspected to have Brugada
 ECG shows – RBBB with coved STE in V1-V3
ECG shows – RBBB with coved STE in V1-V3
- ICD is only successful tx
Long QT syndrome
- Describes an ECG where the ventricular repolarisation (QT Interval) is prolonged
Congenital QT Syndrome
- Mutations in cardiac potassium and sodium channel genes
- 3 main types of congenital long QT (LQT)
- LQT1 – KCNQ1 gene mutation, affects K channel
- Provoked by exercise
- LQT2 – KCNH2 mutation, affects K channel
- Provoked by emotion or loud sounds
- LQT3 – SCN5A mutation, affects Na channel
- Occur at rest or during sleep
- LQT1 – KCNQ1 gene mutation, affects K channel
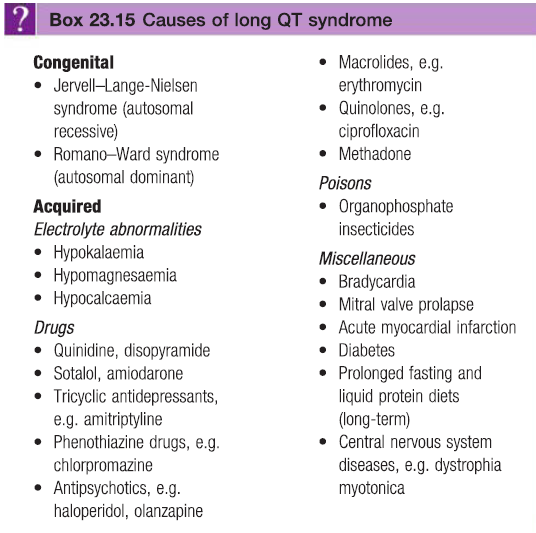
Acquired QTS – most commonly due to bradycardia (see box)
Clinical features
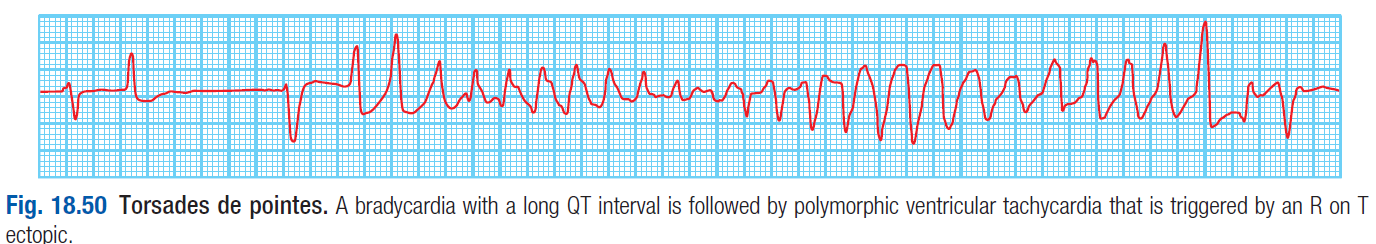
- Syncope and palpitations due to torsades de pointes (a polymorphic ventricular tachycardia)
- Normally terminate spontaneously but can result in VF/sudden death
Diagnosis
- ECG – torsades de pointes seen as rapid, irregular, sharp complexes that continuously change from upright to inverted position
Treatment
- Acquired acute LQT
- Correct electrolyte disturbance (Mg, Ca, K), stop causative drugs
- Maintain HR
- Magnesium sulphate [8mmol]
 Long term management
Long term management
- BB – for LQT1
- Na channel blockers – for LQT3
- Pacemaker
- ICD
Ventricular ectopic beat (VEB)
Etiology
- anxiety, hypokalaemia, hypomagnesaemia, digoxin toxicity, excessive caffeine
Pathogenesis
- VEB is an electrical stimulus of the ventricles which occurs in the ventricles themselves – not from the atria
- Originate from an ectopic location in the ventricles
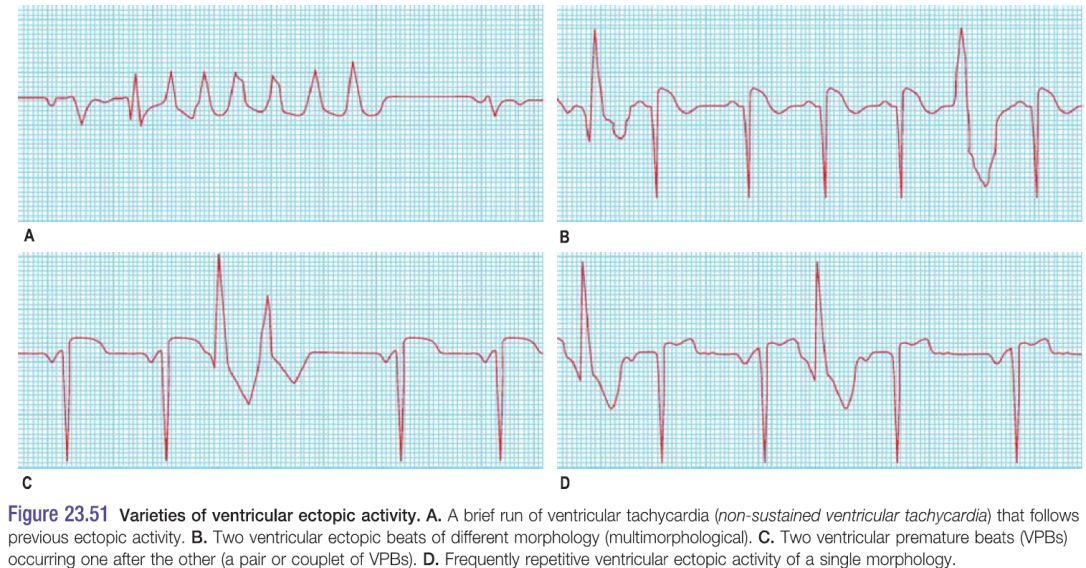
- Caused by groups of pacemaker cells throughout the conducting system that start to operate independently of the normal stimulation. Classified as
- Unifocal – every VEB appears identical (arise from the same ectopic location)
- Multifocal – different VEB morphologies (multiple ectopic sites)
- Following a premature beat there is usually a complete compensatory pause
Clinical features
- Pts complain of extra, missed or heavy beats
- palpitations
- Irregular pulse due to the premature beats
Diagnosis
- ECG
- Absence of P waves before QRS
- Wide, tall QRS >120ms
Treatment
- Tx for otherwise healthy pts not needed
- In VEB pts with troubling symptoms or other heart disease
- Beta blockers
- Catheter ablation
Narrow complex (adenosine)
SVA, multifocal ectopic, AF
Wide complex (lidocaine)
VA, WPW
