1. ACUTE PERICARDITIS
- Normal pericardium contains 50ml of fluid
- Functions – lubricates the heart, limits distension, protects heart from infection/damage, aids filling of ventricles
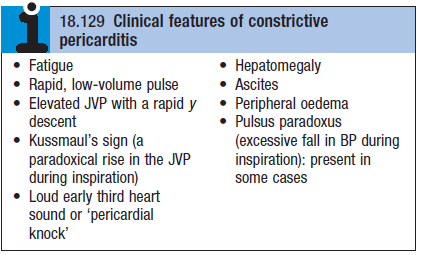
Etiology and Pathology
- See box
- Pericarditis can lead to pericardial effusion
- Can be fibrinous, serous, haemorrhagic, purulent pericarditis
- Fibrinous exudates can lead to adhesion formation (restrictive motion)
- Serous pericarditis can produce a large effusion of turbid, straw coloured fluid with high protein content
- Hemorrhagic effusion – due to malignant disease, esp. ca of breast, bronchus
- Purulent pericarditis – complication of septicaemia, penetrating injury or direct spread of an intrathoracic infection
- Dressler’s syndrome – pericarditis 2o to myocardial/pericardial damage
 Occurs at least 2 weeks after the MI
Occurs at least 2 weeks after the MI
Clinical features
- Retrosternal pain – radiates to shoulder and neck
- Aggravated by deep breathing, movement, exercise
- Low grade fever (LGF)
- Pericardial friction rub – high pitched scratching noise
- Diagnostic of pericarditis
Diagnosis
- Based on CF and history
- ECG
- ST elevation (saddle shaped)
- PR interval depression – specific for acute pericarditis
- FBC – leuko/lymphocytosis due to bacterial/viral infection
- CRP/ESR – inflammatory marker
Treatment
- Simple viral pericarditis – colchicine
- Oral NSAIDs/aspirin for pain
- Purulent pericarditis – ABs
2. PERICARDIAL EFFUSION
- Puts pressure on the ventricles – compromises pumping
- Cardiac tamponade
- Defined as acute HF due to compression of the heart by a large effusion
- CF – ↑JVP, hypotension, pulsus paradoxus, oliguria
- Diagnosis
- ECG – low QRS voltage. Alternating amplitude of QRS due to to-and-fro motion of the heart within the sac
- CXR – globular appearance
- Echo – most useful as directly shows tamponade
- Pericardiocentesis – if infectious cause is suspected e.g. TB
- Needle inserted below xiphoid process, directed upwards towards L shoulder – under echo guidance
- Complications of procedure – arrhythmias, cor. artery damage, bleeding & exacerbation of tamponade
- Treatment
- Tx underlying cause
- If effusion is rapidly forming do pericardiocentesis to avoid tamponade
- Fenestration – for recurring effusion (mostly due to malignancy), creates a ‘window’ within the pericardium
3. TUBERCULOUS PERICARDITIS
- Tuberculous pericardial effusion is a common presentation of AIDS in Africa
- Pericardium becomes thick – leads to constriction and tamponade
- Clinical features – chronic malaise, WL, LGF
- Diagnosis – pericardiocentesis
- Treatment – anti-TB regime
- + 3 months of prednisolone
4. CHRONIC CONSTRICTIVE PERICARDITIS
- Due to progressive thickening, fibrosis and calcification of the pericardium
- Heart is enclosed in a ‘solid shell’ – cannot fill properly
- Often follows an attack of tuberculous pericarditis
- Can also be a complication of viral or purulent pericarditis, haemopericardium, rheumatoid arthritis
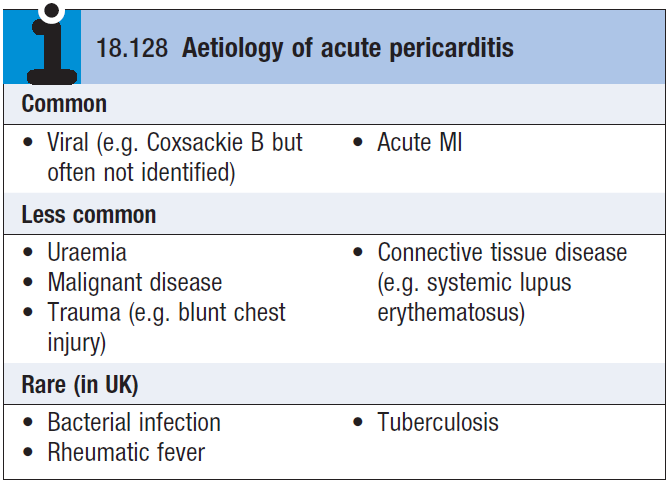
Clinical features – see box
- Symptoms of systemic venous congestion
- AF
- Ascites and hepatomegaly
Diagnosis
- CXR – pericardial calcification
- Doppler echo – to distinguish from restrictive cardiomyopathy
Treatment
- Surgical resection of diseased pericardium – but this is a high risk procedure