1. CHOLECYSTOLITHIASIS
- MC in fat, fertile, forty, flatulent, female
- If symptomatic first line treatment is surgery.
Etiology
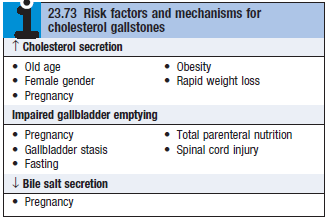
Pathophysiology
- Classified into cholesterol and pigment stones (although majority are mixed composition)
- Cholesterol stones – MC in developed countries
- Pigment stones – MC in developing countries
- Gallstones contain a varying amount of calcium salts – bilirubinate, carbonate, phosphate, palmitate
Cholesterol gallstones
- Cholesterol held in solution in bile by its association with bile acids and phospholipids in the form of micelles
- Admirand’s triangle shows the relationship between lecithin, bile, cholesterol in stone formation.
- Biliary lipoproteins may also have a role in solubilising cholesterol
- In gallstone disease, the liver produces bile that contains ↑ cholesterol
- Because there is either a relative deficiency of bile salts or a relative excess of cholesterol
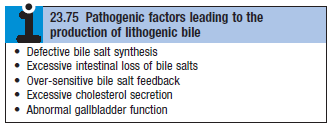 ‘lithogenic bile’ – see box
‘lithogenic bile’ – see box
- Because there is either a relative deficiency of bile salts or a relative excess of cholesterol
- Nucleation factors (which initiate crystallisation of cholesterol in lithogenic bile) determine rate at which crystals form
- Factors favouring nucleation – mucus, calcium, fatty acids
- Antinucleating factors – apolipoproteins
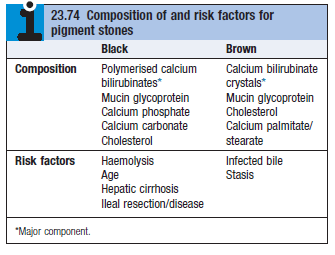
Pigment stones
- Brown + crumbly – MC as a result of bacterial/parasitic biliary infection
- Infection allows bacterial β-glucoronidase to hydrolyse CBR to its free form
- Which then present as calcium bilirubinate
- Black pigment stones – assoc with chronic haemolytic disease
Biliary sludge
- Gelatinous bile that contains numerous microspheroliths of calcium bilirubinate and cholesterol crystals
- Precursor to the formation of gallstones
- Frequently formed under normal conditions, but then is dissolved/cleared by the Gallbladder (GB)
- Fasting, parenteral nutrition, pregnancy are associated with biliary sludge
Clinical features
- Only 10% develop sx of gallstones – biliary pain (colic) or cholecystitis
- Biliary colic – pain occurs suddenly, persists for 2 hours. Non continuous pain.
- MC in epigastrium of RUQ – radiates to R.scapula
- Can mimic oesophagitis, AMI or aneurysm
- Fatty food intolerance, dyspepsia and flatulence
-
- Mucocele (hydropic GB) – if there is slow distension of the GB from continuous sec of mucus
- Can become empyema if gets infected
- Calcium secreted into the lumen of hydropic GB – limey GB
- If calcium salts are precipitated in the GB wall – porcelain GB
- Stone can migrate to the common bile duct (CBD) and cause pain
- Fistula can develop b/w GB and duodenum/colon/stomach (rare – Mirizzi syndrome)
- XR – air in biliary tree
- If stone >2.5cm migrates into gut, it can impact at the terminal ileum
- Causes intestinal obstruction – gallstone ileus (Rigler’s triad for diagnosis)
- Stone impacts in the GB wall and compresses it – pressure necrosis which further gets adherent to CBD wall
- Causes compression and may lead to cholecystocholedochal fistula (rare – Mirizzi syndrome)
Investigations
USS, MRCPLFT
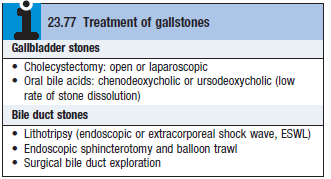
Management
- Asymptomatic gallstones found incidentally don’t need to be treated
- Symptomatic gallstones – laparoscopic cholecystectomy
- If surgery contra-indicated may use endoscopic retrograde cholangiopancreatography (ERCP) but higher risk of complications such as pancreatitis
2. CHOLECYSTITIS
Acute cholecystitis
Pathophysiology
- MC in association with obstruction of the GB neck or cystic duct by gallstone
- Obstruction can also be due to mucus, parasitic worms or bile tumour
- Chemically induced inflammation → GB mucosal damage → release of phospholipase → converts biliary lecithin to lysolecithin (a mucosal toxin)
- Eventually infection occurs
Clinical features
- Pain in RUQ + epigastrium, R.shoulder, non-biliary colic (constant and progressive)
- Difficult to differentiate between biliary colic and acute cholecystitis
- Cholecystitic pain – more severe and prolonged pain, fever, leucocytosis
- Murphy’s sign – pain on inspiration during deep palpation of R.hypochondrium
- Occasional gallbladder mass
- Jaundice (uncommon) – only when stone passes into CBD or Mirizzi syndrome
Investigations
- Peripheral blood leucocytosis
- Minor ^transaminases and amylase (amylase >1000U/L means pain is due to acute pancreatitis)
- XR – radio-opaque gallstones, intrabiliary gas (due to fistula formation into intestine)
- USS – thickened and distended gallbladder
Management
- Medical – bed rest, analgesia (NSAIDs/opiates), ABs (cefuroxime [1.5g/8hrs]/piperacillin), IV fluids
- Some doctors say opioids are contra-indicated
- Surgical – urgent if empyema/perforation develop
DDx
Acute pancreatitis, AMI, cholangitis, renal failure, diabetic ketoacidosis, ectopic pregnancy
Chronic cholecystitis
- Chronic inflam of GB nearly always associated with gallstones
- CF – recurrent attacks of upper abdominal pain, often at night, after a heavy meal
- Patient may recover spontaneously after analgesia and ABs
- Patients usually advised to undergo elective laparoscopic cholecystectomy
- Gallbladder is usually smaller and thicker
