Epidemiology
- Acute ITP – MC in children
- Follows an infection
- Spontaneously resolves within 2 months
- Chronic ITP – MC in adults (females)
- No specific cause identify
- Insidious onset with gradually worsening epistaxis and gingival bleeding
Pathophysiology
- Mediated by autoantibodies (IgG) against the platelet membrane glycoprotein IIb/IIIa (type II HSR )
- Sensitise the platelets, resulting in premature removal from the circulation by macrophages of RES
- Associated with other conditions
- HIV, B-cell malignancies, pregnancy
Clinical features
- Bruising and petechiae
- Epistaxis, gingival bleeding, menorrhagia
- Hematomas in mouth or mucous membranes
- Serious complications – subarachnoid hemorrhage, GIT bleeding
- Spontaneous bleeding occurs with a platelet count <20,000/μL
Diagnosis
- Dx of exclusion
- Exclude possibility of other blood abnormalities except for low platelet count
- Exclude any secondary causes – e.g. leukemia, drugs (quinine, heparin), SLE, HIV
- Lymphadenopathy and splenomegaly are NOT typically present
- BM biopsy – shows increase in megakaryocyte production
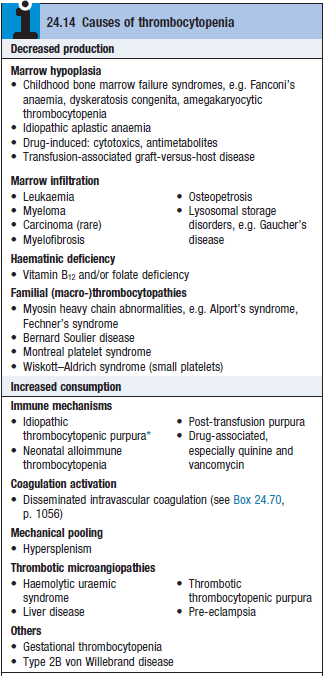
- Ddx – DIC, TTP, HUS
Treatment
- Most stable patients with platelet count >30,000/μL don’t require tx – except for during surgery
- For pts with spontaneous bleeding
- Prednisolone – [1mg/kg/d]
- IV Ig administration – to block antibody receptors on reticuloendothelial cells
- Platelet transfusions
- Splenectomy – if pt has 2 relapses
- Ensure pt is vaccinated due to risk of OPSI
- Rituximab – for patients unresponsive to first line therapy