- Characterised by persistent, progressive airflow limitation – associated with an enhanced chronic inflammatory response to noxious particles/gases
Epidemiology/etiology
- MC in developing countries
- Low socio-economic status
- Ischaemic heart disease, cancer, DM
Environmental factors
- Cigarette smoking
- Occupational exposures – coal dust, silica
- Low birth weight (<2.5kg)
- Recurrent infections
Host factors
- α1-antitrypsin (A1AT) deficiency – leads to ↑neutrophil elastase, which causes destruction of alveolar walls
- Airway hyper-reactivity
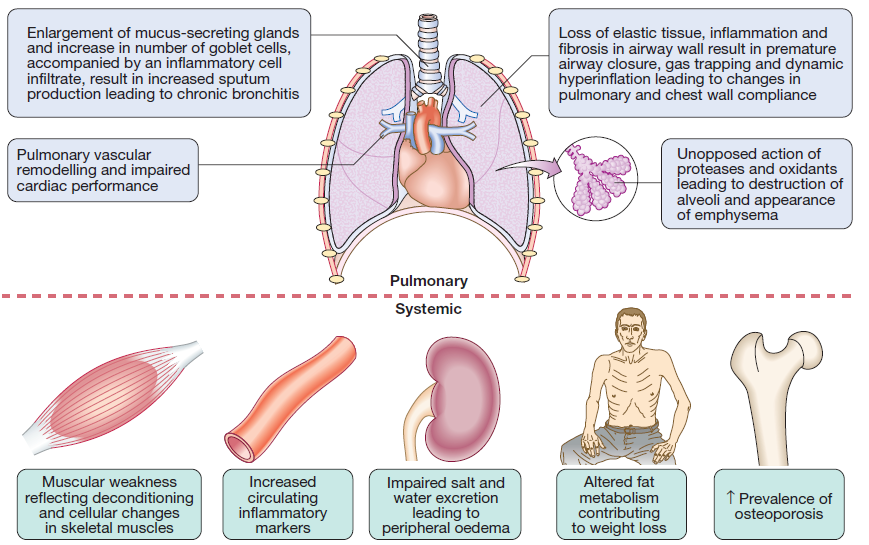
Pathophysiology
Chronic Bronchitis
- Increased number of mucus secreting goblet cells in bronchial mucosa
- Infiltration of the bronchial/bronchiolar walls with acute + chronic inflammatory cells
- Predominantly CD8 – T cells
- Epithelium can become ulcerated and the columnar cells get replaced with squamous cells
- The inflam is followed by scarring and thickening of walls – leads to airway narrowing
- Further progression leads to progressive squamous cell metaplasia and fibrosis – causes airflow limitation
Emphysema – permanent enlargement of airspaces
- Can be centriacinar , paraseptal, panacinar
- Emphysema leads to expiratory airflow limitation and air trapping
- Loss of elastic recoil causes increase in total lung capacity (TCL)
V/Q mismatch is due to 2 main factors
- damage and mucus plugging of smaller airways due to chronic inflam
- rapid closure of smaller airways in expiration due to loss of elastic support
- V/Q mismatch leads to ↓PaO2 and ↑work of respiration
2 types of pts
- ‘Pink puffers’ – MC in pts with emphysema
- Pts have low/normal PaCO2 values due to increasing alveolar ventilation in an attempt to correct their hypoxia
- ‘Blue bloaters’ – MC in chronic bronchitis
- Pts fail to maintain respiratory efforts – leads to rise in PaCO2
- In the long term they become Insensitive to CO2 and rely on hypoxemia to drive ventilation
- Renal hypoxia – leads to fluid retention and ↑erythropoiesis (leads to polycythemia)
- Pt becomes bloated, plethoric and cyanosed
3 main mechanisms of airflow limitation in small airways
- Loss of elasticity due to emphysema – reduces elastic recoil and airways collapse during expiration
- Inflam and scarring – causes airway narrowing
- Mucus secretion – blocks the airways
- Leads to narrowing of airways and air trapping → hyperinflation of lungs, V/Q mismatch, ↑work of breathing and breathlessness
Clinical features
Symptoms
- Productive cough, wheeze, breathlessness
- Infective exacerbations with purulent sputum
- Breathlessness
- Systemic signs – see fig 2
Signs
- Mild COPD – quiet wheezing
- Severe
- tachypnea, prolonged expiration
- use of accessory muscles, pursed lips during expiration
- hyperinflated lungs – barrel chest
- Pink puffers (remain sensitive to CO2) – breathless, pink, NOT cyanosed
- Blue bloaters (insensitive to CO2) – oedematous, cyanosed, don’t seem breathless
Respiratory failure – in later stages of COPD
- PaO2 <60mmHg (<7kPa) or PaCO2 >53mmHg (>8kPa)
Pulmonary HTN
- Cor pulmonale – symptoms of fluid overload secondary to lung disease
- Characterised by Pulmonary HTN and RVH
- Fluid retention + peripheral oedema is due to failure of the hypoxic kidney to excrete Na + water (due to RAAS activation)
- Signs – ↑JVP, ascites, hepatomegaly, ankle pitting oedema
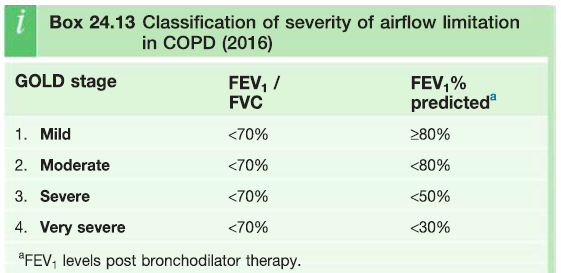
1. DIAGNOSIS
- History of breathlessness and sputum production in a chronic smoker
- Family history of α1-antitrypsin deficiency
Investigations
- LFTs to show evidence of airflow limitation
- ↓ FEV1:FVC
- ↓PEFR
- CXR – hyperinflated lungs, flattened diaphragm,
- Hb – increased due to secondary polycythemia as a result of persistent hypoxemia, >40 RR,
- Sputum exam – S.pneumoniae, H.influenza in acute exacerbations of COPD
- ECG – RVH
- α1-antitrypsin deficiency
2. COMPLICATIONS
Cor pulmonale – pulmonary HTN and RVH
- Due to chronic hypoxemia – which causes constriction of pulmonary arterioles
Respiratory failure – PaO2 <60mmHg or PaCO2 >53mmHg
Type 1 respiratory failure
- Hypoxemia without hypercapnia
- Due to V/Q mismatch
- CO2 is normal/low
- Treatment – O2 to correct hypoxia
Type 2 respiratory failure (mechanical failure)
- Hypoxemia with hypercapnia – due to alveolar hypoventilation
- No VQ mismatch
- Respiratory centre has become desensitised to CO2 levels – so hypoxia is the driving force for ventilation
- Tx – O2 should be given with precaution
- Controlled O2 at 24%
- If PaCO2 continues to rise then give doxapram (respiratory stimulant)
Others
- Arrhythmias – atrial fibrillation
- Secondary polycythemia
- Infection
- Depression
Treatment
1. Smoking cessation
2. Drug therapy
3. Bronchodilators
Beta agonists
- Mild COPD – salbutamol 200mcg every 4-6 hrs (SABA)
- Mod/severe – formoterol 12mcg inhaled bid or salmeterol 50mcg bid
Antimuscarinic
- More prolonged and greater bronchodilation
- Tiotropium 18mcg daily
4.PDE-4 inhibitors – Roflumilast used as an adjunct to bronchodilator therapy
5. Corticosteroids
- Decrease frequency of exacerbation
- Prednisolone 30mg/day x 2 weeks – measure lung function before and after treatment
- If FEV1 increased by >15% then discontinue and give inhaled beclomethasone 40mcg bid
6. Antibiotics and vaccines
- In acute episodes to shorten exacerbation
- Amoxicillin
- Cefaclor 500mg x 3/day
- Cefixime 400mg x1/day
- H. influenza and pneumococcal vaccines
7. Diuretics – loop/thiazide
8. LTOT – long term oxygen therapy
- Indications for LTOT – PaO2 <60mmHg or PaCO2 >53mmHg; polycythemia; pulmonary HTN
- Continuous admin of O2 at 2L/min for ≈15hrs a day – aim to keep saturation >90%
- CPAP (continuous positive airway pressure), CMV (controlled mechanical ventilation), mask
9. Surgery
- Bullectomy – for patients in whom large bullae compress surrounding normal lung tissue
- Improves VQ mismatch
- Lung transplant – for patients with end stage emphysema
10. Additional measures
- a1-antitrypsin replacement
- treatment heart failure
- venesection for secondary polycythemia
Prognosis of COPD – BODE index
