- Respiratory failure – when pulmonary gas exchange fails to maintain normal arterial O2 + CO2 levels
Pathophysiology
Type I Respiratory Failure – V/Q mismatch
- When disease impairs ventilation of part of a lung – e.g. pneumonia/asthma
- Perfusion of that region results in hypoxic and CO2-laden blood entering the pulmonary veins
- Increased ventilation of neighbouring regions of normal lung can ↑CO2 excretion, but cannot augment oxygen uptake because the Hb is already fully saturated
- Admixture of blood from the underventilated and normal region results in hypoxia with normocapnia
- Common causes – pneumonia, acute lung injury, cardiogenic pulmonary edema, lung fibrosis
Type II Respiratory Failure – alveolar hypoventilation ± V/Q mismatch (mechanical failure)
- Caused by conditions that cause alveolar hypoventilation which is insufficient to remove CO2
- This leads to arterial hypoxia with hypercapnia
- Common causes – COPD, Chest wall deformities , respiratory muscle depression ( GBS ), drug overdose
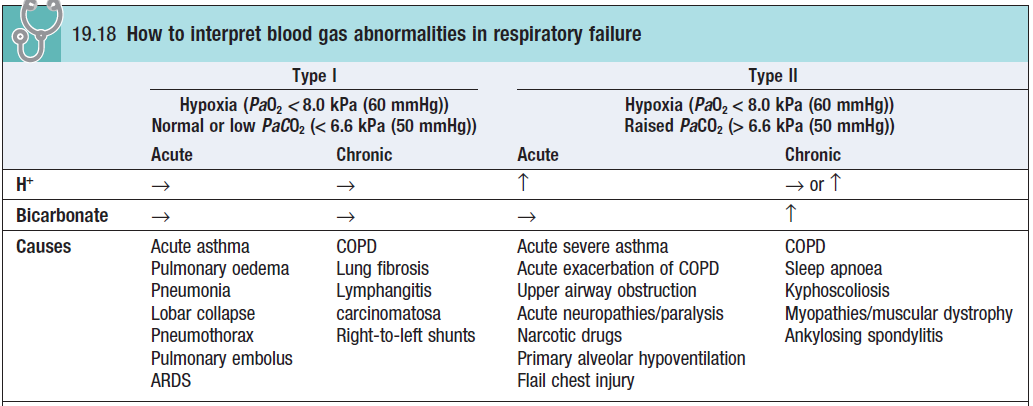
Chronic Respiratory Failure
- COPD is MCC
- Unless there is an acute illness, it remains compensated
- Despite ↑PaCO2, there is no acidosis as kidneys retain bicarbonate
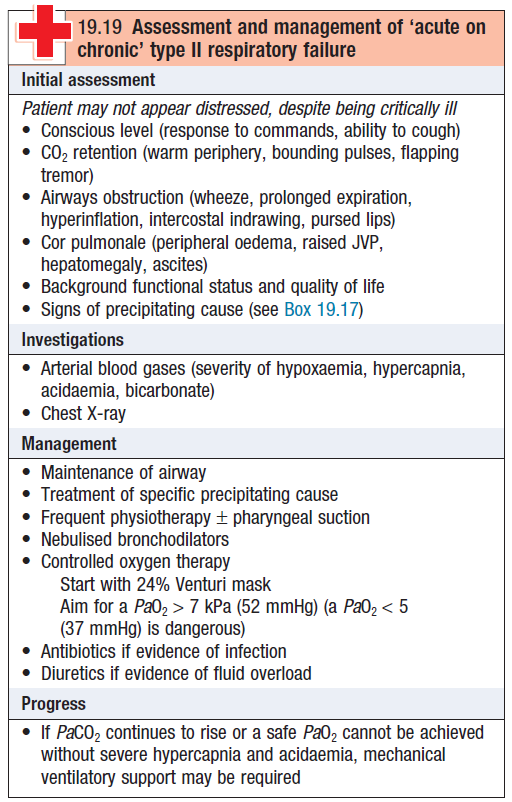
- An acute illness (e.g. exacerbation of COPD) can precipitate acute on chronic respiratory failure
- With acidosis + respiratory disease – can progress to coma
- Patients with chronic respiratory failure have lost their sensitivity to ↑PaCO2
- So they depend on hypoxia for respiratory drive
- These pts are at risk of respiratory depression if given ↑[O2]
Clinical features
Symptoms of hypoxia
- Dyspnea, restlessness, confusion, central cyanosis
- Chronic hypoxia – polycythemia, pulmonary HTN, cor pulmonale
Symptoms of hypercapnia
- Headache, tachycardia, tremor, Papilloedema , confusion, coma
Assessment
- Accessory muscle use, tachycardia, Paradoxical respiration , sweating
