Etiology
- Most common origins of pulmonary emboli are systemic veins
- Pelvic and abdominal veins
- Femoral veins
- Axillary veins
- Clots in veins form due to combination of
- Sluggish blood flow
- Local injury/compression of vein
- Hypercoagulable state
- Emboli can also occur from a tumour, fat (long bone fracture), amniotic fluid, foreign body
Risk factors
- Oestrogen therapy + hormonal replacement therapy
- Pelvis surgery or fracture
- Malignancy
- Myeloproliferative disorders
- MI/stroke
- Age
- BMI >30
- Varicose veins
- Immobility
- Pregnancy
Pathophysiology
- Following PE, lung tissue is ventilated but not perfused (V/Q mismatch)
- Produces an intrapulmonary dead space
- Results in impaired gas exchange
- After few hours, the non-perfused lung no longer produces surfactant
- Alveolar collapse → exacerbates hypoxemia
- Main haemodynamic consequence of PE
- ↓in cross-sectional area of pulmonary arterial bed → ↑pulmonary arterial pressure + ↑RV afterload → ↓CO
- RV ischemia – shown by rise in troponin + creatinine kinase
- Distal embolisation – leads to alveolar haemorrhage, haemoptysis, pleuritic effusion
Clinical Features
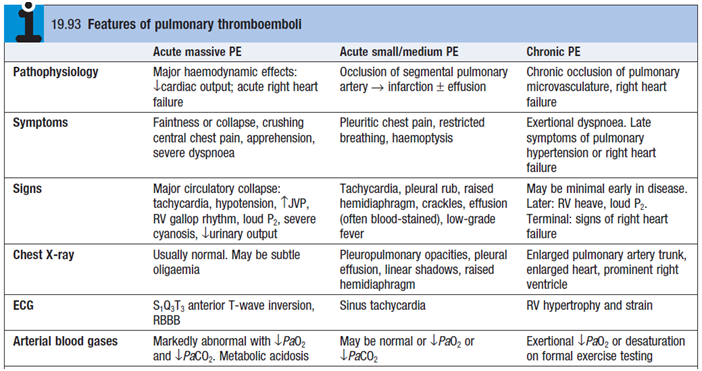
- Sudden onset unexplained dyspnoea
- Pleuritic chest pain, haemoptysis – when infarction has occurred
- Tachypnea, fever
- Pleural rub, coarse crackles
- Hypotension with tachycardia – BAD prognosis
Diagnosis
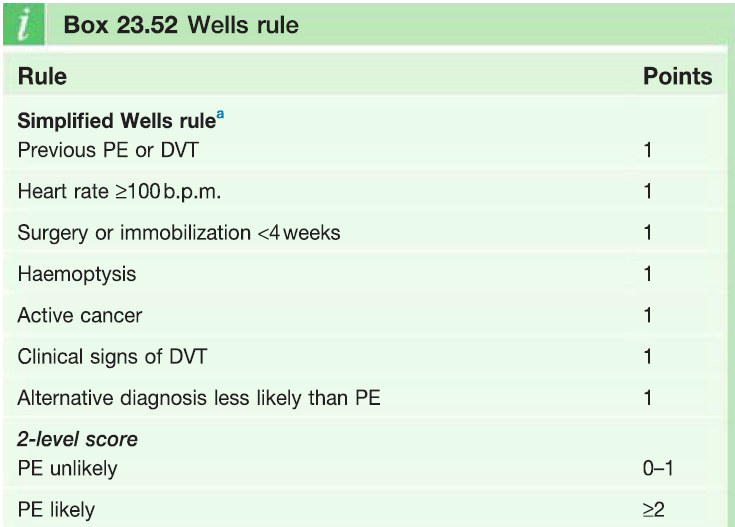
- Clinical status at presentation is divided into ‘high risk’ and ‘not high risk’ – based on presence of shock or hypotension
- If pts are ‘not high risk’ then probability of PE is determined using Wells rule (see table)
- CXR – atelectasis; wedge-shaped pulmonary infarct
- ECG – sinus TC; RA dilation; RAD; RBBB
- ABGs – can be normal or show hypoxaemia
- ↑Troponins
- D-dimer – negative test EXCLUDES PE
- Radionuclide V/Q scanning – with 99mTc scintigraphy
- Shows underperfused areas with normal ventilation
- USS of veins to demonstrate clots
- CT angiogram
- Echo – to show RV dysfunction
- Use Geneva score if Hemodynamically stable
Treatment
Acute management
- High flow oxygen
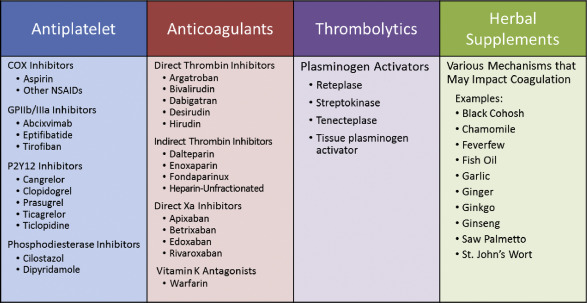
- Anticoagulant – LMWH or fondaparinux
- LMWH (5 days) > rivaoxaban/dabigatran > warfarin
- IV fluids + Inotropic agents – to improve pumping of right heart
- Thrombolysis – to improve pulmonary perfusion
- Indicated in every pt presenting with acute massive PE and cardiogenic shock
- Streptokinase
- Surgical embolectomy
- LMWH (5 days) > rivaoxaban/dabigatran > warfarin
Prevention of further emboli
- Prophylactic anticoagulation
- Warfarin (Vit K antagonist) – for 3-6 months, INR 2-3
- Dabigatran (direct thrombin inhibitor); rivaroxaban + apixaban (Xa inhibitor) – safer than warfarin
- LMWH heparin – for pts with cancer/pregnant
- Vena cava filter in femoral vein