- Uncontrolled proliferation of hematopoietic precursor cells with loss of maturation and differentiation
- The malignant cells (blasts) take over the BM and suppress normal haematopoiesis
- Auer rods – is characteristic of AML
- Linear reddish cytoplasmic inclusions, diagnostic of myeloid lineage
Complications
- Suppression of normal hematopoiesis
- High risk of infx (granulocytopenia), and hemorrhage (thrombocytopenia)
- Metabolic complications
- Hyperuricemia, hyperphosphatemia, hyperkalemia – due to high cell turnover in malignant cells
- Tumour lysis syndrome with ARF – due to urate crystals depositing in tubules (during chemo)
- Allopurinol started and urine is alkalised prior to chemo to prevent this
- Hyperleukocytosis and leukostasis syndrome
- High blast count increases blood viscosity
- Leukostasis syndrome (blasts >50,000/Μl) – altered mental status, respiratory failure, CHF
- MC in AML
- Leukapheresis (removal of WBCs) used to reduce blast count
Diagnosis
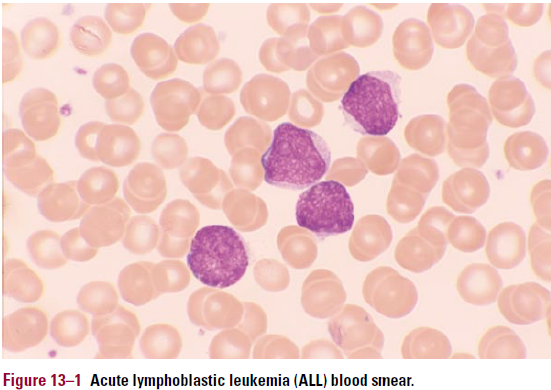
- CBC and blood smear
- BM aspirate
- Cytochemical stains
- MPO – positive in AML
- Sudan black B – positive in AML
- PAS – positive in some ALL
- Flow cytometry
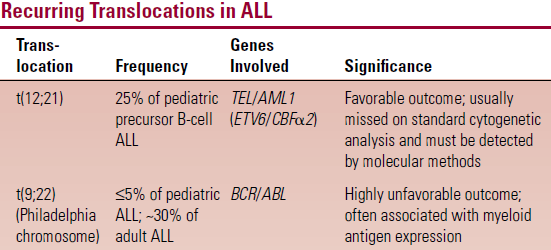
- Cytogenetics
Complications of therapy
- Chemo with cytotoxic agents causes BM aplasis which leads to cytopenias
- Infections – E.coli, K.pneumoniae, Pseudomonas, S.aureus. Fungal infections. Viral (HSV, VZV, CMV)
- Hemorrhage – due to thrombocytopenia. Prophylactic platelet transfusion given
- Other SEs – N, V, alopecia, infertility
- Cytosine arabinoside – cerebellar dysfunction
- Anthracyclines (daunorubicin/doxorubicin) – cardiomyopathy
- Therapy-related AML
1. ACUTE LYMPHOBLASTIC LEUKEMIA
Pathophysiology and Classification
- Clonal proliferation of immature lymphocyte precursors – can be B or T cell precursors (B = 80% of cases)
- FAB classification – based only on morphology, doesn’t mention phenotypes; limited prognostic value
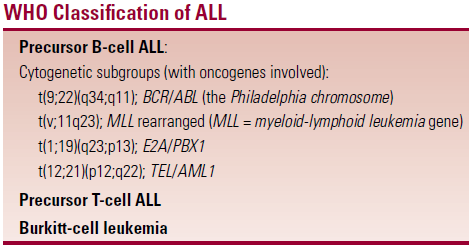
- WHO classification – differentiates based on phenotype (B vs T cell precursors) and cytogenetic anomalies
Epidemiology
- MC in childhood – 1-5 years of age
- Increased risk in children with Down syndrome
- Other predisposing anomalies – Fanconi anaemia, ataxia-telangiectasia
Clinical features
- CF are related to BM infiltration and suppression of normal hematopoiesis
- Pallor, fatigue
- Petechiae and other bleeding signs
- Fever
- Bone/joint pain – due to expansion of medullar cavity by malignant cells
- HSM, lymphadenopathy
- CNS involvement – leukemic meningitis
- BBB decreases penetration of chemotherapy into CSF – provides a ‘pharmacological sanctuary’ for the leukemic cells
 Painless enlargement of testes
Painless enlargement of testes- Precursor T-cell ALL – large mediastinal mass
- May present as respiratory distress
Diagnosis
- Anemia, thrombocytopenia
- Variable WCC – high/normal/low
- Blasts usually found on smear
- Except in aleukemic leukemia
- ↑LDH and UA
- Bone marrow
- Monomorphic population of blasts
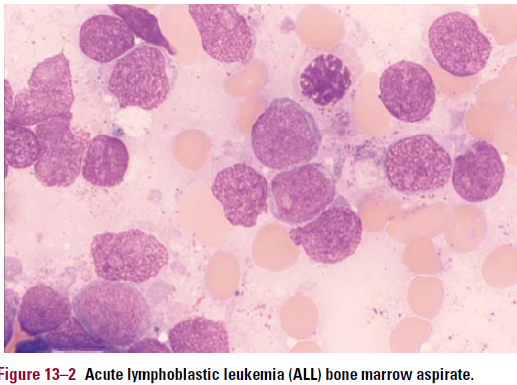 Marked ↓ in normal hematopoietic precursors of all types
Marked ↓ in normal hematopoietic precursors of all types- 50% are PAS+
- Trephine/BM aspiration biopsy
- Immunophenotype
- Precursor B-cell ALL
- Express CD19
- CD10 (cALLA)
- CD34
- TdT+
- Precursor T-cell ALL
- CD2-8
- TdT+
- Burkit cell leukemia (Mature B-cell ALL)
- Presence of Ig (kappa OR lambda)
- CD 19, 20
- Precursor B-cell ALL
Differential diagnosis
- Reactive lymphocytosis – EBV, CMV
- ITP – similar CFs (petechiae, bleeding)
- Aplastic anemia
Treatment
- 3 phases: remission induction, intensification, continuation
- Tx usually lasts 2-3 years.
- Induction – aims to induce remission
- CTST + vincristine
- Plus L-asparaginase or anthracycline in children
- Lasts 4-6 weeks
- CTST + vincristine
- Intensification – higher doses of the drugs in phase 1
- E.g. methotrexate, high dose L-asparaginase, ara-C
- Or combo of vincristine, dexamethasone, L-asp, doxorubicin
- Lasts 6 months
- Continuation
- Weekly methotrexate (po/im) and daily 6-MPU (po)
- Lasts 2 years
- CNS therapy
- Intrathecal methotrexate/ara-C
- Combo with BBB penetrating drugs – dexamethasone
- Intrathecal methotrexate/ara-C
- Neuropenic regime
- I.V fluids, abx, antivirals, chlorhexidine
Complications of tx
- Immediate
- N, V, alopecia, infection, hemorrhage
- Long term
- Avascular necrosis of femoral head due to CTSTs
- Leukoencephalopathy due to methotrexate
- Rare – aggressive brain tumours
