
Mechanisms of immune hemolysis
INTRAVASCULAR – direct complement mediated
- Caused by IgM or IgG Abs that fix complement
- Complement cascade proceeds to the terminal MAC (C5b-9)
- This requires sufficient activation of the system to overwhelm the complement inhibitors
- (C1 inhibitor + C4b binding protein) and the RBC’s own defence mechanisms against comp-mediated hemolysis (CD59 + CD55)
EXTRAVASCULAR – phagocytosis by macrophages of RES
- M of the RES have receptors for the Fc part of IgG and for complement components
- Presence of IgG and complement on RBCs results in phagocytosis of the er
- Occurs mainly in spleen or in liver (Kupffer cells)
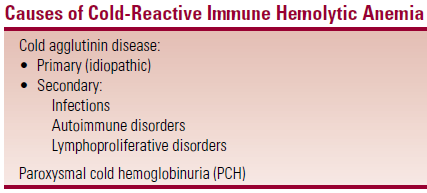
Cold-Reactive Immune Hemolytic Anemia (IHA) – IgM
- Mediated by IgM Abs – which react optimally at 4-18oC
- They bind to cells at the cooler temp of the extremities, fix complement and then dissociate from cell surface after the RBC returns to the warmer temp of central circulation
- The complement components remain on cell surface after Ab dissociates
- IgM Abs can cause intra or extravascular hemolysis depending on titre of Ab (↑titre = intravascular hemolysis)
- Extravascular hemolysis (in the liver) is MC
- IgM Abs are large enough to bridge between RBCs so are able to cause RBC agglutination by themselves (unlike the smaller IgG Abs)
Cold Agglutinin Disease (CAD)
- Primary (idiopathic) CAD
- No obvious precipitating cause.
- MC in older patients – chronic course
- Agglutination of erythrocytes on exposure to cold – MC on fingers, toes, nose, ears
 Associated with CLL/NHL
Associated with CLL/NHL
- Secondary CAD
- Assoc with M.pneumoniae/EBV infections
- Pts are young and otherwise healthy
- Diagnosis
- ↓RCC, ↑MCV, ↑MCHC
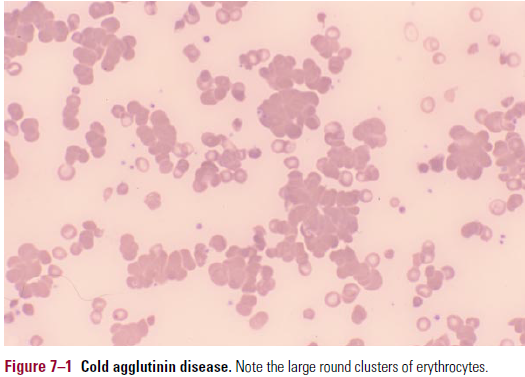
- Smear – large round clusters of RBCs (graininess)
- Re-warming smear to 37oC reverses it
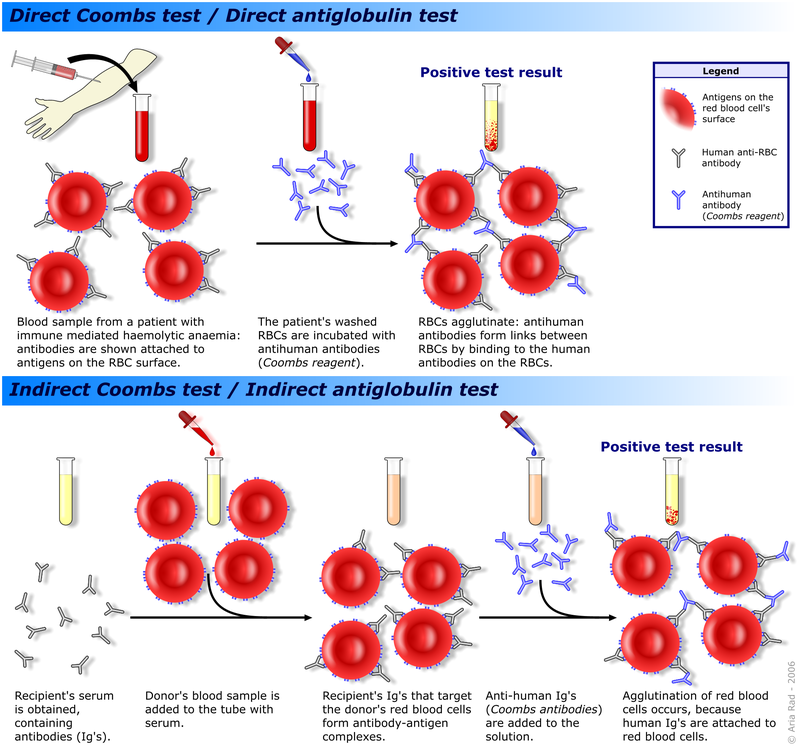
- DAT/Coombs’ test – to detect presence of Ab or complement
- Patient’s cells and Coomb’s reagent (Abs against human IgG/complement) are combined
- If IgG/comp is present on RBC surface, then the cells will combine (+DAT)
- In CAD there is complement on the pt’s RBCs but not immunoglobulin
- IAT/indirect Coombs’ – tests for unexpected anti-RBC Abs in patient’s serum
- Treatment of CAD
- Primary CAD – avoid cold temps. Cyclophosphamide. Plasmapheresis
- Secondary CAD – supportive
Paroxysmal Cold Hemoglobinuria (PCH)
- Characterised by intravascular hemolysis and consequent hemoglobinuria following exposure to cold
- Caused by a biphasic IgG Ab (Donath-Landsteiner)
- Which reacts and fixes comp at cold temps
- Then after re-warming the comp cascade goes to completion with formation of MAC, which causes intravascular hemolysis
 Usually directed against the P blood group Ag
Usually directed against the P blood group Ag
- 3 clinical forms
- Acute form following infection
- Chronic form assoc with tertiary/congenital syphilis
- Chronic idiopathic form
- Clinical features
- Back/leg/abd pain; fever, N, V, headache.
- Dark urine. Severe anemia
- Diagnosis – DAT is positive for complement but not for IgG
- Diagnosis confirmed by the Donath-Landsteiner test
- Pt serum incubated in ice water with group O, P+ RBCs
- Mixture warmed to 37oC
- If cells hemolyse on rewarming then the test is (+)
- Diagnosis confirmed by the Donath-Landsteiner test
- Treatment – supportive; avoidance of cold. Transfusion
Warm-Reactive IHA (MC than Cold IHA)
- Can be primary or idiopathic
- Most cases are due to underlying conditions (see first diagram)
Pathophysiology
- IgG Ab in most cases
- Often react against Rhesus Ag
- RBC destruction is primarily by splenic macrophages (extravascular hemolysis)
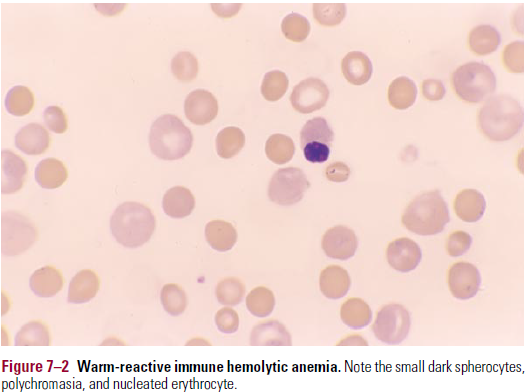
- Hemolysis is partial, resulting in RBCs shaped like spherocytes
- There can be some degree of intravascular hemolysis if there is sufficient comp activation
Clinical features
- Insidious onset of fatigue, weakness and SOB on exertion. Jaundice
 Fulminant (MC in children) – back, leg, abd pain; N, V; dark urine.
Fulminant (MC in children) – back, leg, abd pain; N, V; dark urine.
Diagnosis
- High MCV (due to reticulocytosis)
- Smear – microspherocytes and polychromasia (pic)
- DAT is + for IgG
- DAT- means hereditary spherocytosis
Treatment
- Treat underlying disease
- Corticosteroids – prednisolone [1mg/kg/d]
- Block the M Fc receptors, so prevent phagocytosis
- Decrease Ab production by the spleen
- High rate of relapse
- Splenectomy
- Immunosuppressive – cyclophosphamide, azathioprine
Drug- Related IHA
- Hemolysis is mostly of the warm-reactive type
3 mechanisms of drug-related IHA
- Drug adsorption (penicillin) type
- Drug binds tightly to RBC surface, and an anti-drug Ab reacts with the drug bound to the RBC
- DAT is + for IgG
- Mostly extravascular hemolysis by spleen
- Subacute hemolysis is MC (severe hemolysis is rare)
- Mostly seen with high doses of penicillin
- Neoantigen (immune complex) type
- Complex of drug and anti-drug Ab, which binds to an Ag on RBC
- Ab can be IgG/IgM – often fixes complement
- Then dissociates from cell surface
- Hemolysis is intravascular, usually sudden and severe
- Can be assoc with ARF
- Can occur even with low doses of medication – e.g. cephalosporins, quinine
- Autoimmune (α-methyl dopa) type
- Ab is directed against an RBC Ag, not against the drug itself
- Similar characteristics to idiopathic warm IHA
- Seen in pts taking methyl dopa/levodopa/procainamide
Clinical features
- Insidious fatigue, pallor, jaundice
- Patients with neoantigen type – hemoglobinuria
 Treatment
Treatment
- Discontinue possible medications
- Transfusions for pts with severe hemolysis
