Etiology/Epidemiology
- M>F. Peak incidence at 70yo
- African-American affected more
- Poor prognosis at time of presentation – usually local + distant metastasis
- Cigarettes, chronic pancreatitis, DM, alcohol, chemical exposure
- 5-10% of pts have a genetic predisposition (hereditary pancreatitis, MEN , HNPCC)
Pathophysiology
- 90% of pancreatic neoplasms are Adenocarcinoma – arise from pancreatic ducts
- Involve local structures and metastasise to RLN at an early stage
- Most pts have advanced disease at time of presentation
- Less common – ampullary cancers, originate in ampulla of vater, Better prognosis
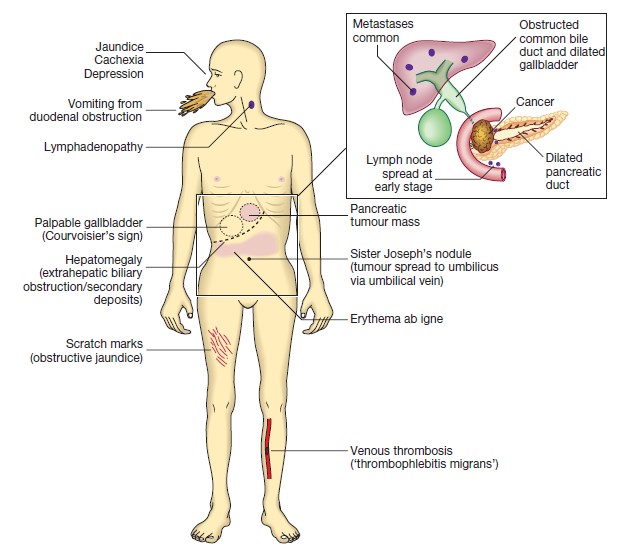
Clinical features
- Asymptomatic for a long time until carcinoma is advanced
- Obstructive jaundice
- Dull epigastric pain, radiates to the back
- Weight loss, anorexia
- Diarrhoea, steatorrhoea
- Lethargy, fatigue
- Courvosier sign – palpable GB with painless obstructive jaundice
- Trousseau sign – migratory thrombophlebitis
- Troisier sign
Investigations
- Blood – ↑conjugated bilirubin
- CA19-9 (good for monitoring), CA-50
- Barium meal – shows widened duodenal ‘C’ loop-pad sign. Reverse 3 sign seen in carcinoma
- US + CT – show pancreatic mass, dilated biliary tree, hepatic metastasis (spiral CT best)
- Endoscopic US with FNAC
- ERCP/MRCP
Management
- Surgical resection – Whipple’s (pancreatico-duodenectomy) for tumours in head of pancreas
- Whipples – choledojejunostomy, pancreaticojejunostomy, gastrojejunostomy
- Chemotherapy with FOLFIRINOX (5-fluorouracil, leucovorin, irinotecan, oxaliplatin
 Improves median survival to 11 months
Improves median survival to 11 months
- Choledochojejunostomy – to relieve jaundice
- Distal pancreatectomy – for body/tail cancers
