- Heterogeneous group of diseases
- Characterised by an increased number of small, mature-appearing lymphocytes in the blood
- The distinction between CLL and non-Hodgkin lymphoma (NHL) depends on presence or absence of peripheral blood involvement, respectively
- Most common type of CLL is the proliferation of small B cells that express CD5 (T-cell associated Ag)
- Other types
B-cell diffuse small lymphocytic lymphoma (SLL has no lymphocytosis)
-
-
- Hairy cell leukaemia (HCL)
- B-cell prolymphocytic leukaemia (B-PLL)
-
1. B-CELL CLL/SLL
Epidemiology
- MC in adults
- United States and W. Europe
- MC in 55-65 year olds
Pathophysiology
- Characterised by slow but persistent accumulation of small lymphocytes
- They are arrested at a functionally immature level
- CLL and SLL cannot be distinguished on examination alone. They are distinguished by presence of lymphocytosis
- CLL if there is lymphocytosis in the blood – >5000 lymphocytes/μL
- SLL if there is no lymphocytosis
- Complications of CLL are considered in relation to 4 factors
- Immunosuppression
- Autoimmune phenomena
- Mass effects
- Transformation to large cell lymphoma
- Hypogammaglobulinemia is common – so pts are exposed to infections e.g. S.pneumoniae
- There are also abnormalities in T-cell number and function – e.g decrease ratio of CD4/CD8 and impaired cell-mediated immunity
Clinical features
- Most pts are asymptomatic at dx – lymphocytosis is detected incidentally at routine CBC
 Symptoms due to anaemia – fatigue, dizziness, dyspnoea
Symptoms due to anaemia – fatigue, dizziness, dyspnoea- Nonspecific symptoms – fever, night sweats, weight loss
- Physical exam can be normal
- MC abnormality is lymphadenopathy
- Mild/moderate hepatomegaly
Diagnosis
- Must be >5000 ly/μL
- Mild anemia or thrombocytopenia
- Hypogammaglobulinemia
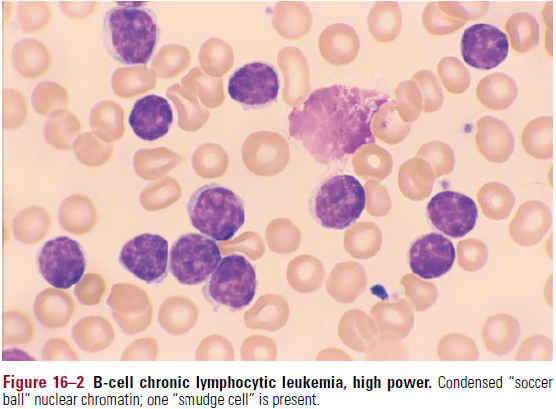
- Blood smear – very characteristic
- ↑number of small mature-appearing lymphocytes
- Nuclear chromatin looks condensed, looks like dense chunks of chromatic surrounded by white spaces (“Soccer ball nucleus”)
- Many disintegrated cells on the smear (smudge cells)
- may be occasional prolymphocytes (larger cells, with less condensed nuclear chromatin)
- Bone marrow
- >30% small lymphocytes
- Infiltration can be nodular, interstitial or diffuse (worst prognosis)
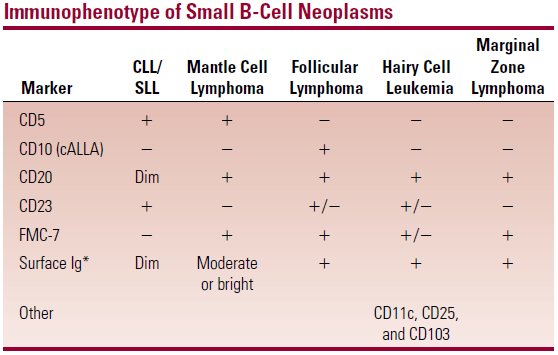
- Immunophenotype
- Expression of CD19, 20, 23, 34 (B-cell markers)
- CD5 (T-cell marker)
- Weak (dim) expression of surface Ig with light chain restriction
- This distinguishes CLL/SLL from mantle cell lymphoma (MCL) which has bright expression of Ig
 Cytogenetics
Cytogenetics
- Chromosomal deletions on – 11, 13, 17
- Deletion on C13 – good prognosis
- Chromosomal deletions on – 11, 13, 17
Differential diagnosis
- Reactive lymphocytosis – MC in younger people. Lymphocytes have more variable appearance
- Leukemic phase of NHL
- SLL – lymphocytes <5000/μL
- MCL – smudge cells are absent. Immunophenotyping by flowcytometry shows difference in surface markers (bright CD20; FMC-7, bright surface Ig, absence of CD23)
- Follicular lymphoma – lys have prominent nuclear folds/clefts
- Prolymphocytic leukemias – larger cell size, less condensed chromatin, different Immunophenotype (CD5 negative)
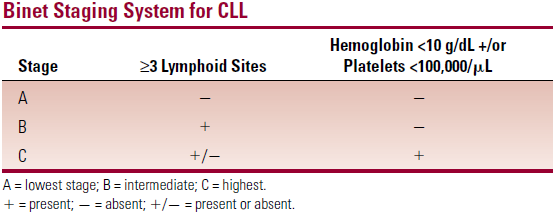
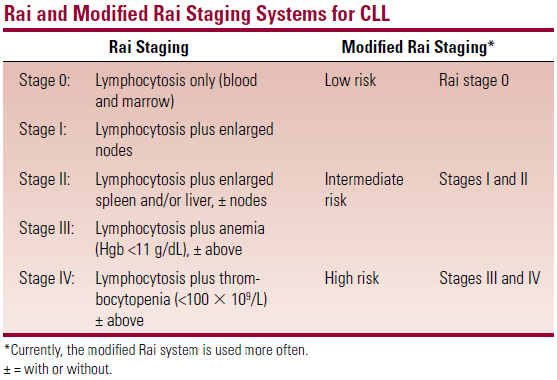
Staging
- The stage in both systems depends on presence of lymphadenopathy and BM compromise
Disease course
- Most pts have indolent disease with long survival
- Complications
- Infections – S.pneumoniae, S.aureus, H.influenza, E.coli, P.aeruginosa
- Autoimmune phenomena – antibodies against blood cells
- Autoimmune HA – warm type. Abs are produced by residual normal B-cells; directed against Rh blood group
- Immune thrombocytopenia
- Evan’s syndrome – simultaneous AIHA and AI thrombocytopenia
- Progression to large cell lymphoma ( Richter syndrome )
- Unresponsive to therapy
Treatment
- Incurable with conventional therapy. Main goal of tx is to control symptoms and maximise quality of life
- Indications for treatment
- To remember tx – RFC
- Rituximab, Fludarabine, Cyclophosphamide
- Progressive systemic symptoms – fever, night sweats, WL
- Progressively worsening anaemia or thrombocytopenia
- AIHA or thrombocytopenia
- Bulky lymphadenopathy that compresses vital structures
- Marked splenomegaly
- Marked lymphocytosis – >150,000/μL
- Treatments
- Alkylating agents – cylcophosphamide, chlorambucil
- CTST – prednisolone (for autoimmune phenomena)
- Purine analogues – fludarabine
- Monoclonal Ab – rituximab (directed against CD20)
