- CML is a myeloproliferative disorder (MPD)
- Clonal stem cell disorders in which regulation of proliferation is impaired, but differentiation and maturation are generally maintained
- Characterised by ↑cell counts – but the increase consist mostly of mature cells
- Different MPDs feature a predominant increase in a single cell line
- CML – granulocytes
- Polycythaemia vera (PV) – erythrocytes
- Essential thrombocythemia (ET) – thrombocytes
- IMF (idiopathic myelofibrosis) – is an exception because it is characterised by cytopenias (dysfunctional fibroblasts)
Epidemiology
- MC in older adults – but can occur at any age
- Possible link to ionizing radiation
Pathophysiology
- Caused by reciprocal translocation between C9 long arm and C22 long arm – t(9;22)
- Philadelphia chromosome
- Results in BCR-ABL fusion gene – which codes for the fusion protein p210
- The normal abl gene codes for a TK enzyme
- But the p210 protein coded by BCR-ABL is more potent TK – acts as an oncogene
- 3 phases
- Chronic, accelerated, Blast crisis
Clinical features
- Mostly discovered as incidental finding
- Fatigue, lethargy, LGF, weight loss
- LUQ discomfort – due to splenomegaly
- Gout – due to hyperuricemia
- Hyperviscosity due to leukostasis
Diagnosis
- ↑WCC – 25,000 – >300,000/μl
- Mild anemia
- Thrombocytosis
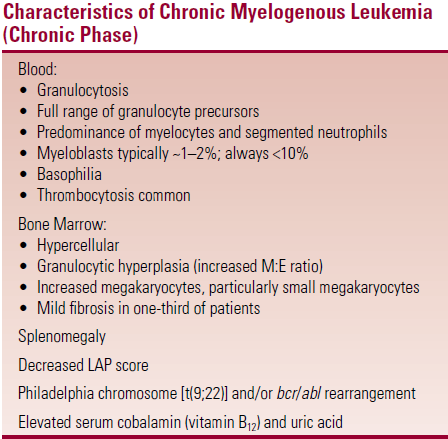
- Blood smear – characteristic (see table + pic)
- ↑LDH + UA + B12
- ↓ LAP
- But can be ↑in infection, treatment or progression to accelerated/blast phase
- Normal LAP score – 20-100
- Also ↓LAP in PNH
- Bone marrow (see table)
- Cytogenetics
- Ph chromosome – 85% of cases
 If case appears to lack Ph then test for t(9;22) and bcr/abl
If case appears to lack Ph then test for t(9;22) and bcr/abl
- t(9;22) – detected by FISH
- bcr/abl rearrangement – detected by PCR
- 9% cases are Ph –ve (poor prognosis)
- Sokal score – prognosis
Differential diagnosis
- Other MPDs – especially ET
- confirm dx by cytogenetics – if Ph present then dx is CML
Disease course
Chronic phase – most patients diagnosed in this phase
- lasts for 3-4 years
- 5% of pts transform within 1st year
Accelerated phase
- Gradual ↑ in blasts in blood/BM, ↑in basophils in blood, or ↑in fibrosis in marrow
- Systemic sx – fever, WL, night sweats
- Short phase – pts either transform to blast crisis or die
Blast crisis
- Defined by presence of >30% blasts in blood/BM
- Mean survival is <3 months
Treatment
Cytotoxic chemotherapy – Switch drug if loss of response
- Hydroxyurea – 2g/d
- DOC to control WCC and systemic symptoms
- Interferon-a – for pts with chronic phase CML
- Decreases proportion of cells in BM that carry Ph chromosome
- SE – flu-like symptoms, athralgia, myalgia, impotence, WL
- BMT – only curative treatment
- Treatment of choice in young pts – BMT should be considered as soon as CML is diagnosed
- TK inhibitors – imatinib [400mg]
- Allopurinol [300mg] – treatment for gout
