- Pneumonia clinically presents as an acute illness with cough, purulent sputum, breathlessness, fever
- With physical/radiological changes consistent with lung consolidation
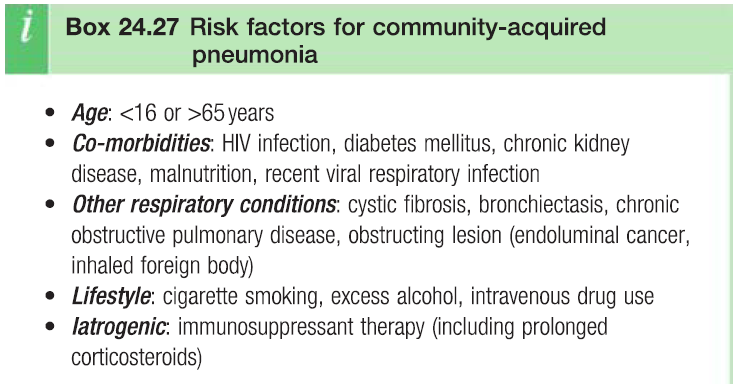
Epidemiology/Etiology
- MC at extremes of ages
- MCC is pneumococcus overall
- Iatrogenic (corticosteroids)
- Other bacteria – M.pneumoniae (young pts) + H.influenza (old pts)
- Viruses – influenza, HSV, VZV, Measles, CMV
- Mostly spread by droplets
Pathophysiology
Lobar pneumonia
- Homogeneous consolidation of ≥1 lobes
- Stages of inflammation
- Congestion – alveoli flooded by exudates, neutrophils + RBCs
- Red hepatisation – fibrin forms on affected lobe (resembles liver)
- Grey hepatisation – lung tissue becomes grey as congestion resolves
- Resolution – restoration of normal architecture of lung
- Most common in elderly
Bronchopneumonia
- Patchy alveolar consolidation associated with bronchial + bronchiolar inflammation
- MC in lower lobes and the young
- Insidious onset
Clinical features
- Cough – dry/productive/haemoptysis. Sputum is rust-coloured in pneumococcal origin
- Dyspnoea– as alveoli become filled with pus and debris
- Fever – swinging fever indicates empyema
- Pleuritic chest pain – and pleural rub
Chest signs – due to consolidation
- Percussion – dull
- Auscultation
- Bronchial breathing
- Coarse crackles
Other signs
- High respiratory rate + pulse rate
- Low BP
- Delirium
Extra-pulmonary features
- Myalgia, arthralgia, malaise
- Myocarditis, pericarditis – MC in M.pneumoniae (atypical pneumonia)
- Abdominal pain, diarrhoea, vomiting
- Labial herpes – MC in pneumococcal
Complications
Immediate
Respiratory failure – PaO2 <80mmHg/6kPa
- Aim for oxygen sat >92%
- Do regular ABGs
Hypotension
- Can be as a result of dehydration and vasodilation due to sepsis
- Treatment with 250ml of crystalline infusion over 15 mins
Medium-term complications
Pleural effusion – inflam of pleura leads to excess fluid production
- Symptoms are not present until fluid is >500ml – ↓chest expansion, dullness, ↓breath sounds, pleural rub
- If fluid becomes infected it can result in empyema
- Treatment – drainage
Empyema – typically presents in patient who has partially recovered but then develops a spike in temperature
- Treatment
- Fluid aspiration – fluid is yellow with low level of glucose
- Chest drainage
- Antibiotics – for 4-6 weeks
- E.g. cefuroxime + co-amoxiclav x 5 days, then metronidazole x 4 weeks (dosages vary according to hospital and patient)
Lobar collapse – most commonly due to sputum retention
Thromboembolism
Pneumothorax
Late complications
Lung abscess – cavitating lesion containing pus
- MCC is S.aureus, K.pneumoniae
- Presents as pneumonia that worsens despite treatment – with purulent sputum, fever, malaise, weight loss
- Investigations
- CXR – shows walled cavity
- ↑ESR + CRP
- Sputum sample
- Bronchoscopy
- Gram negative bacteria most likely to progress to pulmonary gangrene
- Treatment – ABs, drainage, surgical excision (serious cases)
Septicaemia – can result in endocarditis + meningitis
- Pt has poor systemic symptoms (hypotension, spiking fever, hypovolemia)
- Treatment – IV Abs
