Epidemiology
- MC in older people (but can occur in 20-50 year olds)
- MC in women
Pathophysiology
- Clonal hematopoietic stem cell disorder
- Manifests as marked increase in platelet count
- Major consequences are thrombosis and haemorrhage
- Megakaryocytes are only increased but function normally
Clinical features
- Most pts asx at diagnosis – thrombocytosis is usually discovered as an incidental finding
- Microvascular occlusions
- Involve digits – pain, necrosis, gangrene
- Erythromyalgia – redness and burning in digits, which is relieved by aspirin
 Large vessel thromboses
Large vessel thromboses
- MC in lower limbs
- Also in coronary, renal, carotid veins
- Bleeding – GIT, urinary tract, skin, eyes, gums, joints, brains
- Neurologic events – Headaches, TIAs, seizures
Diagnosis
- Platelet count >600,000/μL (most pts have >1000,0000/μL)
- Normal Hb (or mild anemia)
- Mild leukocytosis
- Mild ↑ in LDH + UA
- Criteria dx
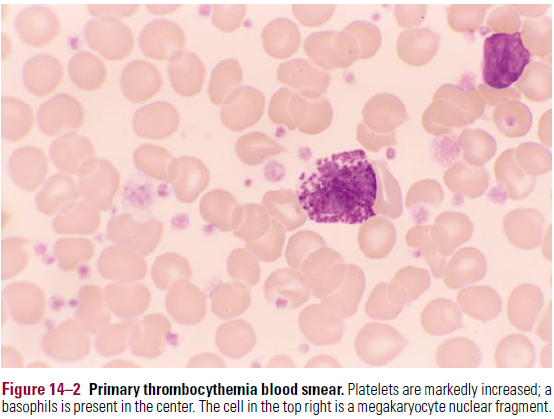
- Blood smear
- Giant platelets, bizarre platelet shapes, megakaryocyte nuclear fragments
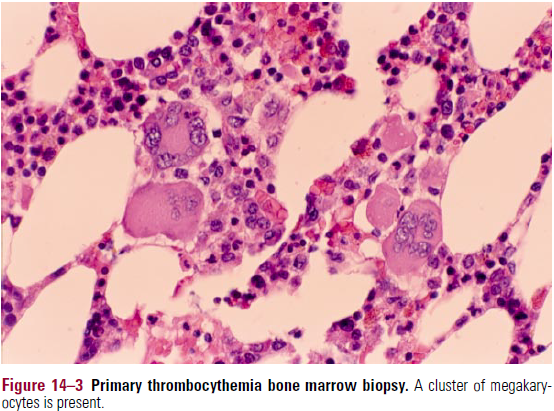
- Bone marrow
- Hypercelluar – marked ↑in megakaryocytes. Clustering of megakaryocytes
- Mild fibrosis may be present (but marked fibrosis MUST be absent for dx of ET)
 Stainable Fe must be present
Stainable Fe must be present
- Cytogenetics
- JAK-2 mutations – 50% of cases
Disease course
- Longest survival out of all of the MPDs
- Rare transformation to MF or AML
- Major threat of thromboembolic events – MC in pts >60
Treatment
- Low dose aspirin – 75-100mg/day
- Hydroxyurea – lowers platelet count
- Anagrelide – 0.5mg tid po
- PDE inhibitor
- Selectively lowers platelet count
- Aim to maintain platelet count <600,000/μL
- Plateletpheresis
- Interferon-a – used in high risk women of childbearing age
