Epidemiology
- Most common Asian countries – Japan, China, Mongolia
- More common in males
- Incidence increases with age
Etiology
- Diet – high salt diet, smoked food, preservatives containing nitrites
Familial – associated with e-cadherin mutation
- Inactivation of p53
- HNPCC
- H. pylori infection → gastritis and decreased acid secretion → gastric atrophy → gastric cancer
Pathology
Gross types
- Cauliflower type
- Ulcerative type
- Leather-bottle (Linitis plastica)
Lauren’s classification
- Intestinal type – favourable prognosis
- H.pylori is the most common cause
- Gland formation and definite cellular architecture
- Gastric mucosa replaced with epithelium that resembles small intestinal mucosa
- Most common in men and the elderly
- Hematogenous spread
- Diffuse type – poor prognosis
- Most common in blood group A, familial type
- Poorly differentiated, signet type
- Early gastric wall penetration
- Lymphatic spread
- Most common in females and young people
- Linitis plastica, ulcerative growth
Depending on depth of invasion
- Early gastric cancer – Japanese Classification
- Involvement of mucosa and/or submucosa only – with or without lymph node involvement
- TNM – T1 + any N
- Advanced gastric cancer – Borrmann’s classification
- Involvement of muscularis and/or serosa – with or without lymph node involvement
WHO histological classification
- Adenocarcinoma (from mucous secreting cells) – Papillary, tubular, mucinous, signet-ring
- Adenosquamous carcinoma
- Squamous cell carcinoma
- Undifferentiated carcinoma
Common site of occurrence
- Prepyloric and pyloric region – most common site
- Body
- Fundus, oesophago-gastric junction
Spread
- Direct spread
- Horizontal submucosal spread along stomach wall
- Vertical spread by invasion to adjacent structures – pancreas, colon, liver
- Lymphatic spread
- Occurs by permeation and embolisation through lymphatics to subpyloric, pancreaticoduodenal, splenic, celiac, aortic lymph nodes
- Later spreads to left supraclavicular lymph node (Virchow’s lymph node)
- Haematogenous spread
- Most often to the liver – causes multiple liver secondaries
- Later to the lungs and bones
- Transperitoneal spread
- Can cause peritoneal seedings – leads to ascites
- Can cause Krukenberg’s tumours in ovaries
Clinical Presentation
- Recent onset of loss of appetite and weight loss, early satiety, fatigue
- Upper abdominal pain and vomiting
- Abdominal mass – nodular, hard, moves with respiration
- Dysphagia
- Jaundice and palpable liver
- Ascites
- (+) Troisier’s sign – palpable Virchow’s node
- (+) Trousseau sign – migrating thrombophlebitis
- Anaemia, cachexia
- Metastatic disease – liver secondaries, ascites, secondaries in ovaries, umbilicus, supraclavicular nodes, lungs and bones
Investigations
- Hb%, haematocrit
- Barium meal – irregular filling defect
- Shows irregular filling defect , loss of rugae, delayed emptying
- Gastroscopy with biopsy
- Endosonography
- US abdomen – liver secondaries, ascites, nodes, ovaries
- FNAC from Virchow’s node
- Laparoscopy – to stage disease
- CT abdomen and thorax – to see size, extent, infiltration, lymph node status, operability
- CA 72-4 (evaluates relapse), CEA, CA 19-9, CA 12-5
Treatment
- Surgery – only curative option
- Preoperative – correction of anaemia, nutrition, fluids and electrolytes
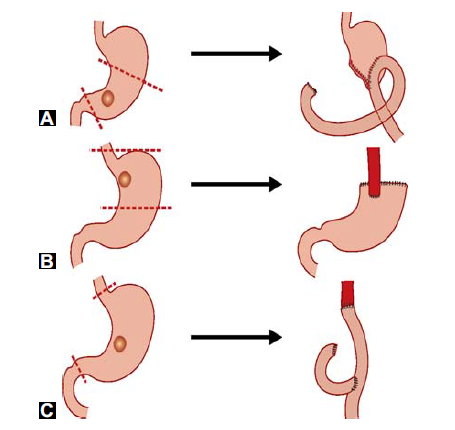
- Growth in pylorus (A) – lower radical gastrectomy with removal of greater and lesser omentum, all lymph nodes, spleen, tail of pancreas and later Billroth II anastomosis (gastrojejunostomy)
- Growth in oesophago-gastric junction (B) – upper radical gastrectomy with removal of spleen, both omentums, lymph nodes and later oesophagogastric anastomosis
- Growth in body or linitis plastica (C) – total gastrectomy with oesophagojejunal anastomisis