1. MEGALOBLASTIC ANAEMIA
- Result from interference in DNA synthesis
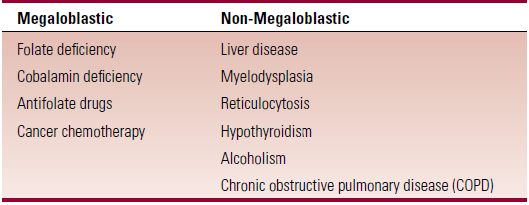
- Megaloblastic anemia – caused by interference with DNA synthesis, due to deficiency of cobalamin or folic acid
- Pernicious anaemia – megalobalstic anemia due to autoimmune chronic gastritis with destruction of parietal cells
Pathophysiology of megaloblastic anemia
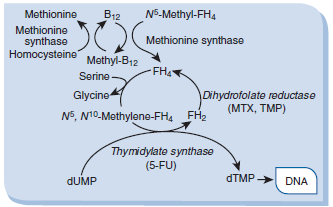
Folic acid
- Required for transfer of methyl groups in many chemical reactions
- Abundant in vegetables, fruits, cereals, dairy
- Absorbed in jejunum
- Daily requirement – 50μg (pregnant – 400μg)
- Primarily stored in the liver
- Deficiency in pregnancy can cause NTDs in fetus
Causes of folate deficiency
- Inadequate diet – ↓fresh fruit+veg; alcoholism
- Malabsorption – celiac disease, SI resection, IBD
- Rare causes – hemodialysis, antifolate drugs, increased requirements (preg, chr hemolytic anemia)
Treatment
- Oral folate supplements – [400-1000μg daily]
- B12 levels need to be normal as folic acid may exacerbate neural degeneration
Vitamin B12
- Sources – meat, eggs, milk, cheese
- Daily requirement – 1μg
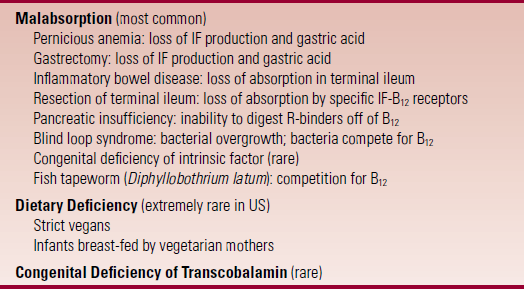
- Most cases of B12 deficiency are due to malabsorption
Steps in cobalamin absorption
- B12 is digested off food protein by pepsin and gastric acid
- The released B12 is then bound to R proteins produced in salivary glands, which block binding of IF
- Panc enzymes release B12 from R proteins, allowing IF to bind
- The B12-IF complex is absorbed in the terminal ileum
- After uptake by the enterocytes of the terminal ileum, the B12-IF complex degrades and transcobalamin II binds B12 to circulate it in the blood and transport it to tissues
2. PERNICIOUS ANEMIA
- MCC of cobalamin deficieny
Etiology/epidemiology
- MC in Scandinavians, British and Irish
- Familial predisposition
- Strong association between PA and other AI disorders e.g. Grave’s and Hashimoto’s, Addisons, vitiligo etc.
Pathophysiology
- PA is an autoimmune chronic gastritis, resulting in destruction of parietal cells and loss of IF production
- Types of antibodies in the serum of a patient with PA
- Anti-parietal cell antibodies
- Anti-IF antibodies
Clinical Features
- Fatigue, lethargy, dyspnoea, faintness, palpitations, yellow tinge to skin
- Glossitis, oral ulceration
- Neurological symptoms
- paraesthesia, numbness, cognitive changes, visual disturbances
- Most advanced cases – hyperreflexia, clonus, Romberg + Babinski
- Demyelination of dorsal and lateral columns of spinal cord, peripheral neuropathy
- Symmetrical impairment of pain, temp, touch sensations; legs involved more commonly
- Triad – absent knee/ankle jerk (LMN), extensor palmaris (UMN)
Lab diagnosis
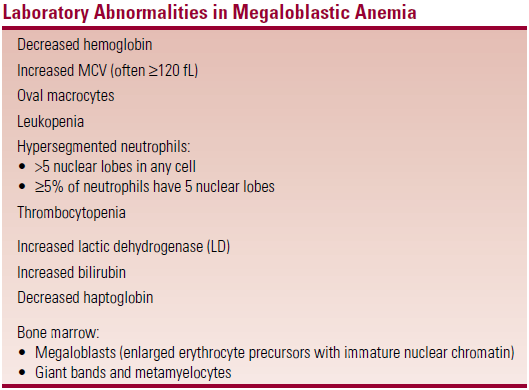
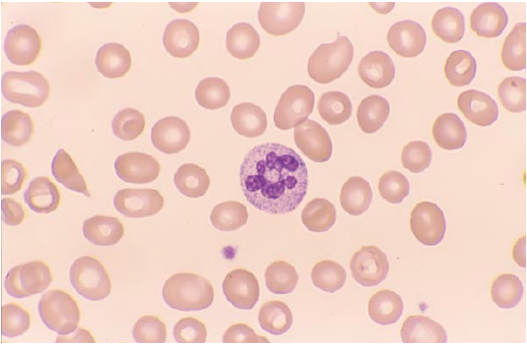
- Key finding – hypersegmented neutrophils (earliest blood finding)
- Increased serum LDH and BR due to marked intramedullary hemolysis
- Bone marrow – hypercellular, increased erythroid precursors
- Megaloblasts are large erythroid precursors with an immature (open) nucleus
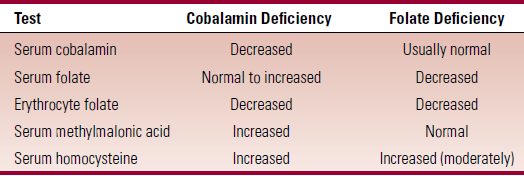
- Biochemistry (table)
- Increased MMA (methylmalonic acid) is very sensitive for B12 deficiency, increase homocysteine
- Schilling test – standard method to diagnose PA once B12 deficiency is confirmed
- Radiolabelled B12 is given orally and a large dose of B12 is given i.m. Urine collected for 24hrs
- Amount of radioactivity in urine indicates how much B12 was absorbed oraly
- Recovery of <6% B12 in urine indicates malabsorption
- If initial value is ABNORMAL, then IF is given together with radiolabelled B12
- Increase in the amount of B12 absorbed during this stage indicates PA
- Serum analysis – anti-parietal cell Abs; anti-IF Abs
- Other causes of B12 deficiency – metformin, coeliac disease, crohns
Treatment
- Parenteral therapy
- Hydroxycobalamin [1mg x 3 weeks, then 1mg every 3 months] – checks levels on day 3/5/7
- Rapid response to therapy
- Reticulocytosis in 2 days, Hb rises after 1 week, hypersegmented neutrophils disappear in 2 wks, BM shows disappearance of megaloblasts within few days
