Epidemiology
- Colorectal ca is 3rd leading cause of cancer death in each sex
- Peak incidence – 70yrs
Etiology
- Ageing – dominant risk factor
- Hereditary conditions – FAP, HNPCC
- Environmental and dietary – high fat diet, processed meats, smoking, alcohol
- Inflammatory bowel disease – Crohn’s disease, ulcerative colitis
- Other risk factors – male sex, history of other cancers
Pathogenesis
- Results from the accumulation of multiple genetic mutations arising from 2 major pathways
Loss of Heterozygosity pathway (development of FAP)
- Mutations
- Mutations in APC gene and KRAS gene
- Loss of DCC tumour suppressor gene
- Mutation of p53
- This pathway carries a poor prognosis
Replication Error Repair pathway (development of HNPCC)
- Germline mutations in enzymes involved in repairing errors that occur normally during DNA replication
- These genes are – hMSH2 + SH6; hMLH1 + LH3; hPMS1, + MS2
- These replication errors accumulate and can be detected in microsatellites of repetitive DNA sequences
- Leads to microsatellite instability
- This pathway carries a better prognosis
Classification – WHO histological classification
- Adenocarcinoma – 90%
- Mucinous adenocarcinoma
- Signet ring cell carcinoma
- Small cell carcinoma – rare, very poor prognosis
- Squamous cell carcinoma
- Undifferentiated carcinoma
Staging – Duke’s Criteria
- A – growth limited to rectal wall
- B – invasion through rectal wall penetrating the muscular layer, but not involving lymph nodes
- C – involvement of lymph nodes
- D – widespread metastases
Clinical features
- Can be asymptomatic
- Change in bowel habits – diarrhoea, constipation, tenesmus
- Rectal bleeding
- Mucus in stools – spurious diarrhoea
- Anal, perineal, sacral pain (invasion of sacral plexus)
- Mass may be palpable on per rectal exam
- Ascites, liver secondaries
Investigations
- Digital rectal exam
- Barium enema
- Sigmoidoscopy and colonoscopy – biopsy can be made
- Transrectal US – pre-operative staging of rectal carcinoma
- MRI – imaging modality of choice to stage the disease
- The mesorectal fascia is a layer of connective tissue enclosing the perirectal fat surrounding the rectum
- It extends from the beginning of the rectum to levator ani
- Contents – perirectal fat which contains the superior rectal artery and vein, lymph nodes and vessels
- Important landmark in rectal cancer staging – forms the circumferential resection margin (CRM)
- The distance between the tumour and the mesorectal fascia is predicative of whether complete resection will be possible
- A margin of <1cm denotes that local recurrence is likely
- The mesorectal fascia is a layer of connective tissue enclosing the perirectal fat surrounding the rectum
Treatment
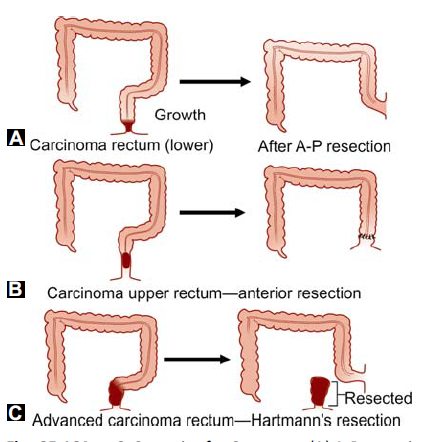
Surgery (see pic)
- Abdomino-perineal resection (Miles operation)
- For low rectal cancers
- Removal of the anus, rectum and part of sigmoid colon
- Remaining part of the sigmoid is brought out as end colostomy
- Anterior resection
- For growths in the mid and upper rectum
- Followed by colorectal anastomosis
- Hartmann’s operation
- Used as a palliative procedure in elderly patients who are not fit for major resection
- Resection of rectosigmoid colon with closure of the recto-anal stump, and formation of an end colostomy
Radiotherapy
- Adenocarcinoma responds well to radiotherapy
- Can be used postoperatively to downgrade the tumour